You know, there’s a question that lingers for a lot of people when they first hear the diagnosis: Can hidradenitis suppurativa kill you? And honestly? It’s a fair thing to wonder. When you’re dealing with something that causes deep, painful nodules, wounds that won’t heal, and months — sometimes years — of flare-ups… You start thinking in bigger terms. Not just “how do I fix this?” but “what is this doing to my body long-term?”
So let’s start simple. Hidradenitis suppurativa (HS) is a chronic skin condition. Technically, it’s considered a disorder of the sweat glands and inflammation of hair follicles, mostly in areas like your underarms, groin, buttocks, or breasts. But putting it that clinically feels… hollow. Because if you’re living with it, you know it’s more than some dermatology blurb. It hurts. It lingers. It can change how you move, how you dress, and how you even talk to people.
This article will break that down — not just the risks, but why they happen, how you can lower them, and how people are treating HS today in real-life, real-body ways. You’ll find insights on causes, stages, treatments, and even mental health, because — let’s be real — chronic illnesses like this don’t just affect your skin.
1. What Is Hidradenitis Suppurativa?

So, what is hidradenitis suppurativa? The name sounds clinical — and it is — but at its core, HS (also called acne inversa) is a chronic skin condition marked by deep inflammation under the skin. Painful lumps, draining tunnels (sinus tracts), and thick, rope-like scars tend to form in sensitive areas and often come back.
It’s more than skin-deep — classified as an inflammatory disease, HS involves immune system responses and possibly your microbiome. The exact cause isn’t clear, but a mix of genetics, hormones, and factors like obesity, smoking, and environment likely play a role.
2. Who Gets Hidradenitis Suppurativa?
Statistically? It tends to show up after puberty, often between the ages of 18 and 40, and it’s more common in women. There’s also some data pointing to higher prevalence in Black and Hispanic populations, though underdiagnosis and diagnostic delay make this tricky to pin down.
Risk factors include:
- A family history of HS (genetics does seem to matter)
- Metabolic syndrome (which is linked to things like type 2 diabetes, liver dysfunction, and non-alcoholic fatty liver disease)
- Autoimmune or inflammatory diseases like inflammatory bowel disease
- Smoking (huge one)
- Obesity or rapid weight gain
And while it’s not officially contagious or caused by poor hygiene (let’s clear that up right away), it still carries social stigma. Probably because the symptoms look… raw. Angry. And the smell from persistent drainage during HS flares doesn’t help. It’s one of those conditions that impacts quality of life in deeply personal, often invisible ways.
3. Where Does Hidradenitis Suppurativa Usually Happen?

Here’s a table to make this a bit easier:
| Commonly Affected Areas | Why These Areas? |
| Underarms | Lots of apocrine sweat glands |
| Groin and inner thighs | Friction, moisture, and hair follicles |
| Buttocks | Sitting pressure, sweat glands |
| Under breasts | Heat, weight, and skin folds |
| Around the anus | Friction + moisture combo |
Some people only get mild outbreaks in one or two spots. Others, especially in more severe cases, see it spread to multiple areas, sometimes with interconnected lesions and fibrotic tissue that never quite heals.
1. Wait — Is HS the Same as Acne?
Good question. They’re related but not the same. HS isn’t typical acne — it’s not caused by clogged pores or excess sebum. That’s why standard acne treatments don’t usually work. Instead, HS involves deep skin inflammation.
plus those sinus tracts and chronic abscesses. So while it’s sometimes called acne inversa, that label is misleading — HS behaves more like a chronic inflammatory disease than a teenage skin issue.
2. How Is It Diagnosed?
In clinical practice, HS is often diagnosed by:
- Visual examination of lesions
- Medical history and pattern of flares
- Rule-outs for infections or other skin diseases
There’s no blood test or definitive scan — which leads to lots of misdiagnoses, especially early on. Some people go years before they hear the actual name for what they’re dealing with.
4. Can Hidradenitis Suppurativa Kill You? Understanding the Mortality Risk
Okay, so let’s just go ahead and tackle it. Can hidradenitis suppurativa kill you? Like, literally — is this a condition that could cost you your life?
It’s not the easiest question to ask. Or answer. But it matters.
HS is rarely fatal on its own. The skin condition itself — the abscesses, sinus tracts, the scarring — doesn’t directly cause death. However… and this is where nuance comes in… the secondary complications and chronic inflammation associated with HS can raise your mortality risk over time.
There has been data — limited, but growing, suggesting that people with long-term, untreated HS may have higher chances of developing other health issues. Particularly those tied to systemic inflammation, like:
- Cardiovascular disease (including myocardial infarction or heart attack)
- Cerebrovascular accidents (aka strokes)
- Severe infections (think: bacterial infections turning into sepsis)
- Metabolic syndrome
- Liver dysfunction, including non-alcoholic fatty liver disease
- And — very rarely — a type of skin cancer known as squamous cell carcinoma
So, technically? Yes — there’s a path, albeit a long and unusual one, where untreated HS could eventually lead to something life-threatening. But it’s often a complex web of indirect causes.
Let’s Break That Down
| Type of Risk | Connection to HS | Fatal Potential |
| Infection | Open wounds + sinus tracts can get infected, especially in deep tissue | Yes, if it leads to sepsis or other life-threatening infections |
| Cancer | Chronic inflammation over decades can rarely lead to squamous cell carcinoma | Yes, but very rare |
| Heart Disease | Chronic systemic inflammation = higher risk of cardiovascular death | Indirect but real risk |
| Liver Disease | Associated with metabolic issues and inflammation | Potentially fatal in late stages |
| Suicidal Ideation | Tied to chronic pain, social isolation, and mental health decline | Non-physical but critical mortality factor |
Now — and this really matters — these complications don’t affect everyone with HS. In fact, many people manage the condition for life without ever facing these extreme outcomes. But the risk increases when severe HS goes untreated, especially in Stage III cases with persistent drainage, thick scarring, and chronic abscesses.
5. So… How Often Does HS Actually Lead to Death?
Honestly? There’s no giant pile of statistics to point to. HS is underreported, and it’s usually not listed as a direct cause of death even when it contributes.
But studies like those from Olmsted County and large-scale reviews in clinical practice suggest that HS does correlate with higher overall mortality rates, particularly in individuals with comorbidities like diabetes, obesity, or autoimmune conditions.
So again, the answer isn’t a hard yes or no. It’s more like: “Probably not… but maybe, if it’s complicated and ignored for too long.”
And that “maybe” is enough to make proactive care worth it.
6. Complications That May Increase Health Risks
Alright, let’s get into the gritty stuff. You might wonder, “If HS itself doesn’t usually kill you, what exactly makes it dangerous?”
The truth is — the danger lives in the complications. Some are physical, some emotional, and others… well, a mix of both. Let’s talk about the ones that matter most.
1. Infections & Sepsis: When Wounds Go From Painful to Perilous
You probably already know this if you’ve had an HS flare that didn’t heal right — these aren’t ordinary skin bumps. They can go deep. And if bacteria get trapped in those sinus tracts, it can spiral fast into a bacterial infection or worse, cellulitis or sepsis.
🔸 Pro Tip: If a wound becomes hot, swollen, red, and you feel feverish or dizzy, don’t wait. Seek medical attention right away. That’s your body screaming that something’s off.
2. Squamous Cell Carcinoma: A Rare But Real Threat
This one’s scary, but rare enough that you don’t need to panic. Still — it’s worth knowing: long-standing, severe HS, especially in the anogenital area, can in rare cases lead to squamous cell carcinoma — a type of skin cancer.
Why? Chronic inflammation over decades can alter how cells divide and repair. Think of it like the body getting so used to being inflamed, it forgets how to respond correctly.
Some cases documented in medical literature have shown fatal outcomes from cancer that was originally rooted in HS lesions.
It’s not common. But it’s not impossible.
3. Fistulas and Tunneling: More Than Skin Deep
HS doesn’t always stay on the surface. In Stage II and III, it can form tunnels under the skin, connecting abscesses through pathways called fistulas. These aren’t just painful — they can also:
- Worsen infections
- Trap bacteria
- Damage deeper tissue
- Require surgical interventions
Sometimes they grow so dense that they form fibrotic tissue, which makes healing even harder. It’s like your body is trying to patch things with scar material, but ends up creating a thick maze of pain.
4. Reduced Mobility and Diminished Quality of Life
If you’ve ever had HS under your arms or between your thighs, you know how something as basic as walking can become an ordeal. Over time, scarring to life areas — places where your skin needs to bend, stretch, move — can dramatically reduce your quality of life.
Some patients report:
- Avoiding social situations due to odor or drainage
- Missing work during flares
- Sexual avoidance or shame
- Ongoing chronic pain from scarred areas
And all of that? It adds up — slowly eroding the everyday sense of normalcy.
✅ Quick Recap: Common HS Complications Worth Watching
| Complication | Risk Level | What to Watch For |
| Infection/Sepsis | High | Fever, red-hot skin, swelling |
| Squamous Cell Carcinoma | Rare but severe | Non-healing wounds, growing ulcers |
| Fistulas/Tunneling | Moderate to high | Painful lumps under the skin, interconnected abscesses |
| Mobility Issues | Common | Pain during walking or arm movement |
| Mental Health Decline | High | Isolation, depression, loss of interest in life |
7. Mental Health and Emotional Toll of HS
So, we’ve talked about the body — the infections, the scarring, the silent risks. But what about your mind?
It’s almost too easy to overlook how much hidradenitis suppurativa affects your mental health — because most of it doesn’t show up on a scan. There’s no MRI that captures what it feels like to isolate yourself from friends because you’re afraid of leaking or odor. No lab test can detect the dread that builds before a date, a work presentation, or even just a beach day.
But the pain is real. And for many? It’s heavier than the physical part.
In fact, studies — and real people — keep pointing to the same thing: people living with HS are far more likely to experience:
- Depression
- Anxiety disorders
- Body image struggles
- Suicidal ideation
1. Why Is HS So Hard Emotionally?
Let’s be honest — the symptoms can be brutal. Chronic abscesses, persistent drainage, thick scarring, and constant discomfort don’t exactly set the stage for components of health.
But beyond that, there’s this ongoing feeling of loss: of normalcy, of spontaneity, of physical comfort. And for many, especially in more severe cases, HS flares disrupt daily life. That uncertainty? It takes a toll.
2. A Personal Note (Fictional but Familiar)
One patient once described it like this:
“It’s like waking up every day and having to negotiate with your own body — where can I go, what can I wear, who can I talk to… based on whether or not I’m leaking through my clothes.”
That level of exhaustion — decision fatigue, shame, anticipation of judgment — isn’t something you bounce back from with just a painkiller.
3. Link Between Pain and Suicidal Thoughts
Unfortunately, chronic pain and suicidal ideation often go hand in hand. HS brings both — the physical sting of flares and the psychological weight of living around them.
A study found that people with hidradenitis suppurativa were twice as likely to have a diagnosed psychiatric disorder, and three times more likely to report suicidal thoughts compared to the general population. These aren’t just numbers — they’re quiet battles playing out every day in real lives.
Pro Tip: 👉 If you ever find yourself thinking it’s too much — please, talk to someone. Your pain is valid. And there’s more help out there than most people realize. Therapy, support groups, antidepressants, mindfulness, peer chats — you don’t have to handle this alone.
4. How to Manage Mental Health With HS?
There’s no perfect blueprint, but here’s a layered approach that might help:
| Mental Health Strategy | How It Helps | Access Point |
| Cognitive Behavioral Therapy (CBT) | Reframes negative thoughts around body image and pain | Psychologist or online therapy apps |
| Pain Psychologists | Specializing in chronic pain + mental health interaction | Often via pain clinics |
| Support Groups (Online/In-Person) | Reduces isolation, normalizes your experience | Reddit, Facebook, HS-specific platforms |
| Mindfulness/Meditation | Helps manage anxiety spikes during flares | Free apps like Insight Timer, Calm |
| Psychiatric Medications | Treats depression or anxiety at the chemical level | Through primary care or psychiatry |
8. What Causes HS and Who Is at Risk?
Alright — deep breath. Let’s step back and ask: Where does this even come from? Why does hidradenitis suppurativa happen to some people and not others?
Well… it’s complicated. There’s no one-size-fits-all trigger, but we know a mix of genetics, inflammatory pathways, hormones, and lifestyle choices all seem to play a role.
So while it’s frustrating (understatement of the year) to not have a single root cause, let’s break down what researchers do know.
🔸 1. Genetic Predisposition
About 30–40% of people with HS have a family history of it. That’s a big clue. Some research suggests a link to mutations affecting inflammatory cells or skin structure, but it’s still being mapped out.
🔸 2. Hormonal Imbalances
HS often flares during:
- Puberty
- Menstrual cycles
- Pregnancy
- Menopause
This points to a hormonal component — possibly tied to androgens or how hair follicles react to hormonal shifts.
🔸 3. Obesity and Weight Management
Adipose tissue (fat) produces pro-inflammatory signals, which may worsen HS. More skin folds also = more friction and sweating, increasing the chance of follicle inflammation and chronic abscesses. Weight management isn’t a cure — but it can help with symptom control.
🔸 4. Smoking
Probably the strongest behavioral link. Smokers are significantly more likely to develop HS, and flares tend to be more severe. The exact reason’s still debated, but may involve nicotine’s impact on sweat glands and immune system regulation.
🔸 5. Environmental and Lifestyle Factors
Things like tight clothing, poor air quality, stress, and even gut health (hello, microbiome-based therapeutics) may influence flares. It’s a surprisingly whole-body disease.
Pro Tip: 👉 If you’re noticing small, recurring lumps or under-skin “pimples” that don’t behave like acne — especially in friction zones — talk to a dermatologist early. Early intervention can prevent years of scarring.
9. How Hidradenitis Suppurativa Progresses Over Time
Doctors like to organize things. And fair enough — when you’re dealing with a complex condition like HS, it helps to have some kind of roadmap. That’s where the Hurley staging system comes in. It splits hidradenitis suppurativa into three main stages, based on how severe it gets and how much of your body it affects.
But here’s the truth: most people don’t feel like they “fit” into just one stage all the time. Some parts of your body might be at Stage I, while others — especially areas with repeated flares — may have escalated to Stage III. It’s not always linear, and it’s definitely not one-size-fits-all.
Still, it’s a useful way to understand the progression of HS and why early treatment matters.
The Hurley Stages of Hidradenitis Suppurativa
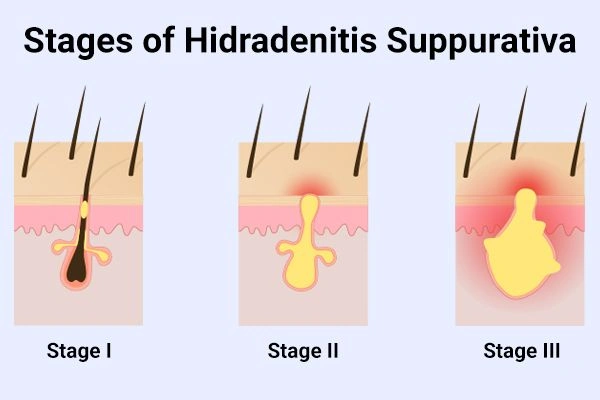
| Stage | Symptoms | What It Feels Like | Treatment Urgency |
| Stage I | Single or multiple painful bumps; no tunnels (sinus tracts) or scarring yet | It comes and goes. You hope it’s just acne. | Low to moderate, but early care helps |
| Stage II | Recurrent lumps, abscesses, tunneling, some fibrotic tissue | Things start to connect under the skin. Pain lingers longer. | Moderate — time to seek consistent care |
| Stage III | Widespread lesions, persistent drainage, extensive scarring, sinus tracts | Movement hurts. Clothes hurt. Socializing feels impossible. | High — may require surgical interventions |
10. When Does HS Become Dangerous?
It’s usually in Stage III, where the skin’s been through repeated flares, where chronic inflammation has had years to dig in. That’s when we start seeing:
- Severe infections
- Thickened, rope-like scars
- Immobility in affected areas
- And rarely — squamous cell carcinoma
Also? That’s when many people hit their emotional breaking point. Physical damage is one thing. The constant negotiating with your body and your life is another. That’s why comprehensive treatment plans — involving dermatologists, mental health support, even nutritionists — are vital at this stage.
Pro Tip: 👉 If you’re bouncing between flare-ups and never seem to fully heal, that’s a sign you might be transitioning to Stage II or III. Don’t wait. Early interventions can prevent scarring, and sometimes that’s the line between chronic pain and manageable symptoms.
Can You Stop HS From Progressing?
Sometimes, yes. While HS isn’t “curable” in the traditional sense, a lot of patients slow or halt its progression with a combination of:
- Biologics (like Humira)
- Weight management
- Laser hair reduction in affected zones
- Anti-inflammatory treatments (including antibiotics, corticosteroid injections)
- Careful tracking of HS flares and triggers
And honestly? Just being taken seriously by your doctor early on can make a huge difference.
11. Treatment Options to Prevent Complications
So let’s get practical. When you’re dealing with something that’s painful, recurring, emotionally exhausting, and potentially life-altering, the biggest question becomes: What helps?
Thankfully, hidradenitis suppurativa treatments have evolved. And while no single solution works for everyone (wish it did), there’s a growing list of approaches to help you find relief — and avoid severe complications down the line.
Let’s break them into tiers.
1. Common Treatments for Hidradenitis Suppurativa
| Treatment Type | Examples | When It’s Used |
| Topical Medications | Clindamycin, resorcinol | Mild HS, early flares |
| Oral Antibiotics | Doxycycline, rifampin + clindamycin combo | Moderate HS, bacterial infections |
| Hormonal Therapy | Anti-androgens (spironolactone), oral contraceptives | Female patients with hormonal flares |
| Biologics | Adalimumab (Humira), infliximab | Moderate-to-severe HS with systemic inflammation |
| Surgical Options | Incision & drainage, wide excision, laser therapy | Refractory or Stage III HS |
| Emerging Therapies | Botulinum toxin injections, microbiome-based therapeutics | For targeted or resistant cases |
2. Which Treatments Work Best?
Honestly, it depends. But here’s what some dermatologists and real patients say:
- Biologics have been game changers for many, especially in slowing down new HS flares
- Laser hair reduction (especially diode laser) reduces follicular inflammation in common HS zones
- Surgical interventions, while intimidating, often offer long-term relief when medications fail
- Combining meds with lifestyle modifications (like a healthy diet, stress reduction, smoking cessation) improves outcomes significantly
3. How Long Until You See Results?
Fair question — and a frustrating one. Because with HS, progress often feels slow.
- Antibiotics may help flares within a few weeks
- Biologics can take 2–3 months to show consistent improvement
- Surgical recovery depends on depth and location — could be weeks to months
The key is ongoing management. HS isn’t a “try one thing” situation. It’s about building a comprehensive treatment plan that adapts over time. And sticking with it, even when it’s tedious.
Pro Tip: 👉 Keep a flare journal. Track symptoms, food, stress levels, and cycle timing. It sounds basic, but it gives your care team data to fine-tune your plan. Plus, it helps you feel a little more in control.
12. Managing Daily Life With Hidradenitis Suppurativa
Let’s get something out of the way: Lifestyle modifications won’t “fix” HS. This isn’t one of those “just eat kale and meditate” situations. But they can reduce flare-ups, make symptoms more manageable, and help you feel a little more in control of your body again.
Because when you’re living with something that doesn’t always respond predictably to meds or surgery, even the small stuff — what you eat, what you wear, how you move — starts to matter.
And honestly? Lifestyle changes are often the missing layer in a lot of comprehensive treatment plans.
1. Skincare Habits That Actually Help
You might already feel like your skin is under attack, so the last thing you want is irritation from your routine. Here’s a gentler approach:
| Tip | Why It Helps |
| Use antibacterial washes like chlorhexidine or benzoyl peroxide | Keeps sweat glands and hair follicles clean |
| Avoid scrubbing or using loofahs on active lesions | Reduces irritation and the risk of spreading bacteria |
| Stick to loose, breathable fabrics | Reduces friction and sweat buildup in vulnerable areas |
| Shave with care (or consider laser) | Shaving can trigger inflammation of hair follicles — laser hair reduction is often safer for HS |
2. Food, Triggers, and the Whole “Healthy Diet” Thing
Here’s where it gets frustrating: there’s no one HS diet that works for everyone. But a lot of patients — and emerging research — suggest that diet recipes plays a role in symptom control, especially in reducing inflammatory pathways.
Common triggers people report:
- Dairy
- High glycemic foods (white bread, sugar, soda)
- Brewer’s yeast (found in beer, bread, and soy sauce)
- Red meat or processed meats
Now, that doesn’t mean you have to go full vegan keto tomorrow. Just… observe. Try an elimination diet for a few weeks. Keep a journal. Your skin will tell you what it loves and hates, eventually.
3. Movement, Exercise, and Body Confidence
When you’re dealing with chronic abscesses and thickened, rope-like scars, exercise can feel like a cruel joke. But movement helps reduce inflammation, manage metabolic syndrome, and even improve mental health.
Try low-friction options like:
- Swimming
- Stationary cycling
- Walking with moisture-wicking gear
- Yoga (just maybe skip hot yoga if sweat is a major trigger)
Also, if you avoid the gym because of HS symptoms, you’re not alone. Many people with HS experience social isolation due to the fear of odor or visible lesions. But comfort can come from routine and clothing choices that help you feel more covered and secure.
4. Support Matters More Than You Think
There are entire online communities built around HS support — Reddit threads, Facebook groups, private forums. You’ll find tips, venting, and just people who get it. Sometimes you don’t need advice. Just validation.
Pro Tip: 👉 Try moisture-absorbing powders (like zinc oxide blends) for friction areas. Especially between thighs or under the breasts. It’s not a cure, but it can seriously reduce flare triggers.
13. Warning Signs That Require Urgent Attention
Here’s the thing no one likes to think about — but should: sometimes, hidradenitis suppurativa flares aren’t just inconvenient. They’re actually dangerous.
And that’s where the original question — Can hidradenitis suppurativa kill you? — circles back in again. Not directly, not often. But life-threatening infections, uncontrolled bleeding, or signs of systemic inflammation can put you in real danger if ignored.
So let’s break it down clearly.
1. Emergency Symptoms of HS
If you’re living with HS, you already know the day-to-day discomfort. But these signs go beyond the usual:
| Symptom | Why It’s Dangerous |
| Rapid swelling and spreading redness | May indicate cellulitis or deep skin infection |
| Fever, chills, or confusion | Could mean sepsis, a medical emergency |
| Severe, uncontrolled pain | Could signal an abscess has ruptured internally |
| Bleeding that won’t stop | Especially in surgical or high-pressure areas |
| Sudden fatigue or shortness of breath | Rare, but may indicate a systemic infection or cardiovascular issue |
2. Flare-Up vs. Emergency: How to Tell
| Situation | Likely a Flare | Time to Go to ER |
| Painful lump that returns every month | ✅ | ❌ |
| Drainage, but no fever or swelling | ✅ | ❌ |
| Abscess that doubles in size overnight, red-hot to touch | ❌ | ✅ |
| General fatigue during your period | ✅ | ❌ |
| Fever + chills + draining wound | ❌ | ✅ |
Sometimes, especially if you’re used to pain, it’s easy to ignore these signs. But infections tied to HS have, in rare cases, led to hospitalization and even death if left untreated.
This is where HS edges into truly serious territory. And it’s why you should never feel guilty about “overreacting” — because when it comes to signs of life-threatening infections, there’s no such thing.
3. Urgent Care vs. Emergency Room?
If you’re unsure where to go, here’s a quick guide:
| Symptom | Go to Urgent Care | Go to ER |
| Mild flare-up with drainage | ✅ | ❌ |
| High fever + swelling | ❌ | ✅ |
| Wound won’t close after a week | ✅ | ❌ |
| Sudden spreading rash or dizziness | ❌ | ✅ |
Pro Tip: 👉 If you’ve been prescribed antibiotics before and you notice they suddenly stop working during a flare, that’s a red flag. You may be dealing with a resistant infection. Don’t wait — call your provider or head to urgent care.
14. Strategies for Reducing Long-Term Risks
Untreated HS doesn’t just stop at the skin. It can sneak below the surface — literally and figuratively — into places you wouldn’t expect. That’s why, even if the condition isn’t directly fatal, the potential consequences of letting it spiral are serious.
Things like:
- Chronic pain that interferes with work, relationships, and daily living
- Thickened, rope-like scars and fibrotic tissue that limit mobility
- Sinus tracts that become tunnels of ongoing infection
- Delayed diagnosis leading to non-alcoholic fatty liver diseases, peripheral vascular disease, or even squamous cell carcinoma (a rare type of skin cancer linked to HS in some severe cases)
1. Why Early Diagnosis Changes Everything?
Many people with HS wait years — sometimes a decade or more — before getting properly diagnosed. It’s often misread as acne, boils, or just recurring skin infections. That diagnostic delay? It’s dangerous.
The sooner it’s recognized, the sooner a comprehensive treatment plan can begin. That includes:
- Keeping inflammatory cells in check
- Preventing tunneling and scarring
- Avoiding dangerous infections
- Monitoring for any signs of skin cancer in long-term wounds
2. Regular Screenings & Checkups Matter
Living with HS often means juggling more than one health issue. Studies have shown links between hidradenitis suppurativa and:
- Liver dysfunction
- Inflammatory bowel disease
- Metabolic syndrome
- Increased risk of myocardial infarction (heart attack) or cerebrovascular accident (stroke)
So don’t just treat the skin. Keep up with:
- Dermatology visits (every 3–6 months for moderate/severe HS)
- Blood panels to watch for inflammation, liver issues, and cholesterol
- Screenings for squamous cell carcinoma, especially in long-term, non-healing wounds
3. Here’s What a Long-Term HS Management Plan Might Include:
| Element | Why It Matters |
| Weight management | Reduces friction, sweat, and systemic inflammation |
| Healthy diet | Helps modulate inflammation and metabolic risk |
| Psychiatric support | Prevents isolation, anxiety, and psychiatric disorders linked to chronic illness |
| Dermatologic therapy | Controls flares, prevents sinus tracts |
| Surgical interventions (if needed) | Can eliminate chronic problem areas and reduce persistent drainage |
| Microbiome-based therapeutics (emerging) | Targets bacterial imbalance in the skin environment |
It’s not just about symptom relief. It’s about slowing progression and preserving your quality of life — even as your body changes.
Pro Tip: 👉 If you’ve had the same inflamed area for over a year with little healing, ask your doctor for a biopsy. Chronic lesions in HS can (rarely) transform into squamous cell carcinoma, a type of skin cancer. Early detection could save your life.
Final Thoughts
What is hidradenitis suppurativa? The name sounds clinical — and it is — but at its core, HS (also called acne inversa) is a chronic skin condition marked by deep inflammation under the skin. Painful lumps, draining tunnels (sinus tracts), and thick, rope-like scars tend to form in sensitive areas and often come back. It’s more than skin-deep — classified as an inflammatory disease, HS involves immune system responses and possibly your microbiome.
The exact cause isn’t clear, but a mix of genetics, hormones, and factors like obesity, smoking, and environment likely play a role. While it’s not contagious or caused by poor hygiene, its impact on daily life can be profound. Early diagnosis and proper treatment can help manage symptoms and reduce flare-ups.
Frequently Asked Questions
1. What is considered severe hidradenitis suppurativa?
Usually, Hurley Stage III — when there are multiple interconnected sinus tracts, chronic abscesses, and deep scarring that may limit mobility or cause ongoing infections.
2. How can I clear up hidradenitis suppurativa flare-ups?
Clearing up a flare might involve antibiotics, warm compresses, anti-inflammatory medications, and sometimes a corticosteroid injection. Keeping the area clean and dry also helps.
3. What foods should I avoid with HS?
Common triggers include dairy, high-sugar foods, refined carbs, and brewer’s yeast. Try cutting one at a time and observing how your skin reacts.
4. Does stress make hidradenitis suppurativa worse?
Yes. Stress can activate inflammatory pathways and trigger HS flares — even if everything else stays the same.
5. What is the best pain relief for hidradenitis suppurativa?
Depends on the stage. Over-the-counter NSAIDs help early on; for severe chronic pain, a dermatologist may suggest topical anesthetics, oral medications, or surgery.
6. Can hidradenitis suppurativa turn into cancer?
In rare cases, squamous cell carcinoma has developed in long-term, non-healing HS wounds. This is why monitoring and biopsies are important for chronic lesions.
7. What is end-stage hidradenitis suppurativa?
This refers to Hurley Stage III — widespread inflammation, scarring, and sinus tracts with little remission between flares. Surgical intervention is often necessary.
8. How do you mentally cope with having HS?
Therapy, support groups, journaling, antidepressants (if needed), and connecting with others who understand. Mental health is part of HS treatment, not separate from it.
9. Does hidradenitis suppurativa make you fatigued?
Yes, chronic inflammation can lead to body-wide fatigue. Sleep disturbances from pain also add to exhaustion.
10. Should I be worried if I have hidradenitis suppurativa?
Worried? No. Aware and proactive? Absolutely. With proper treatment, HS is manageable, and serious complications are rare with early care.



