An osteoarthritis flare-up is a temporary worsening of joint pain, stiffness, and swelling caused by inflammation or overuse of affected joints. These flares can last anywhere from a few days to several weeks, depending on triggers like weather, activity level, or stress. While unpredictable, they’re manageable with the right lifestyle adjustments and treatments.
Imagine waking up one morning and your knees feel heavier, stiffer — like they’ve aged overnight. You’re not weak or unlucky; it’s just your joints signaling for extra care. Each flare carries a message, and learning to decode it can make every future episode shorter and easier to handle.
So, how long do osteoarthritis flare-ups last — and what can you do to shorten them? In this guide, we’ll explore the science behind flare-ups, identify common causes, and share proven strategies to ease discomfort. Keep reading to discover how to move through pain with awareness, strength, and lasting relief.
I. How long Do Osteoarthritis Flare-Ups last? (Science Behind the Pain)
Maybe you’ve had days where your knees feel perfectly manageable, and then suddenly — out of nowhere — they’re on fire. That’s the hallmark of an OA flare-up, a temporary surge in symptoms that can make even gentle movement feel like resistance training.
A. The Inflammatory Response in OA
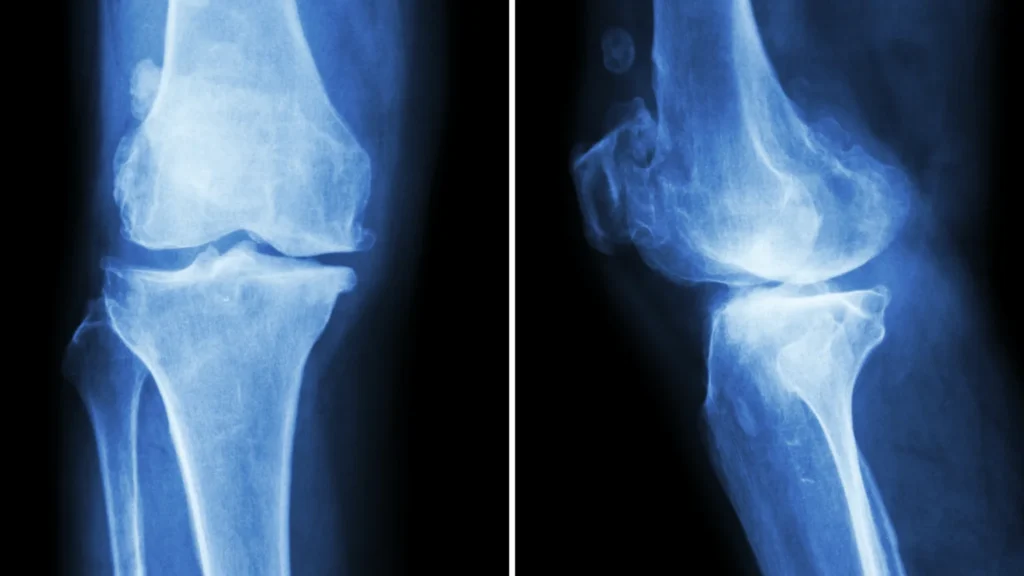
Osteoarthritis isn’t just about cartilage wearing down. It’s an active biological process where the synovium (the joint lining) becomes inflamed.
Researchers from University College London and the Cleveland Clinic have shown that the release of pro-inflammatory molecules — especially interleukin-6 and TNF-alpha — accelerates cartilage breakdown. This inflammation increases joint fluid and swelling, putting pressure on nerves and reducing the smooth glide of movement.
In short, the joint’s delicate ecosystem — cartilage, bone, synovial fluid — goes out of balance. The joint’s cartilage loses elasticity, and bone spurs may start forming as the body’s way of compensating. Ironically, these little “repairs” can cause even more friction.
There are also systemic layers. People with secondary osteoarthritis (caused by another condition like psoriatic arthritis, ankylosing spondylitis, or juvenile idiopathic arthritis) may have heightened immune sensitivity. Their bodies may release inflammatory markers even in mild stress situations.
B. How Pain Signals Work During a Flare
During a flare, your nerves become extra chatty — nerve sensitization kicks in, meaning even light pressure feels exaggerated. This isn’t “in your head”; it’s the result of chemical changes around the nerves. The Short-Form McGill Pain Questionnaire (SF-MPQ-2) has shown that people often describe OA pain as “burning,” “aching,” or “shooting.”
Some studies (like those from Arthritis Care & Research) suggest that psychological and sensory processing differences — the way your brain interprets discomfort — play a big role in flare intensity. That’s why two people with similar joint damage might report wildly different experiences.
Comparing Baseline vs Flare-Up Pain Responses
| Feature | Baseline OA | During Flare-Up |
| Pain Type | Dull ache, manageable | Sharp, pulsating, often radiating |
| Swelling | Minimal | Noticeable fluid buildup |
| Movement | Stiff but possible | Restricted or painful |
| Emotional Impact | Low-level fatigue | Anxiety, sleep disturbance |
When inflammation finally cools down, pain slowly recedes — though not always back to zero. That lingering stiffness you feel afterward? It’s often a sign of micro-inflammation or early joint damage that might need a bit more musculoskeletal care.
II. 10 Common Causes of Osteoarthritis Flare-Ups (and How to Manage Each One)

Sometimes, osteoarthritis flares feel random. You wake up, and your degenerative joint disease just… decides it’s mad today. But usually, there’s a reason — or ten of them. Recognizing your personal triggers helps you shorten recovery time and even prevent future flares.
1. Overuse or Repetitive Movement
- Cause: Overloading joints through repetitive strain — long walks, stair climbing, or lifting.
- Fix: Adjust your exercise intensity. Add recovery days. Work with a physical therapist or occupational therapist to improve joint mechanics and posture.
It’s easy to underestimate how small, repeated motions build up over time. Even something as simple as carrying groceries every day can spark an OA flare if your body’s already tired.
Taking short breaks, stretching, and using ergonomic supports can reduce microtrauma and help maintain joint cartilage health.
2. Weather Changes (Barometric Pressure Drops)
- Cause: Sudden dips in air pressure cause tissues to expand, irritating already inflamed joints.
- Fix: Keep joints warm with compression sleeves, use heat therapy, and practice range-of-motion exercises indoors.
Many people notice pain spikes right before it rains — that’s the barometric pressure effect in action. The shift causes joints to subtly swell, which increases tension and inflammatory arthritis activity.
If you can, plan indoor stretches or warm baths during cold fronts. Even a warm compress can quiet the ache before it escalates.
3. Stress & Poor Sleep
- Cause: Elevated cortisol increases inflammatory markers and nerve sensitivity.
- Fix: Try mindfulness, breathwork, or light yoga before bed. Magnesium-rich foods or guided relaxation apps help too.
When stress builds, your body’s natural Treg cell balance gets disrupted, which can worsen inflammation. It’s not just emotional — your immune system physically changes under strain.
Sleep acts like a reset button. Deep rest allows the joint’s cartilage to recover micro-damage and reduces next-day pain sensitivity.
4. Weight Gain or Inflammatory Diet
- Cause: Added load on joints and systemic inflammation from processed foods.
- Fix: Focus on anti-inflammatory nutrition — leafy greens, berries, omega-3s, olive oil, turmeric. Drink enough water; even mild dehydration worsens joint stiffness.
Extra body weight doesn’t just stress the knees and hips — it also increases the release of cytokines that inflame tissues. Over time, that adds up to faster cartilage breakdown.
Even small improvements — like swapping refined carbs for whole grains — can ease pain levels and improve patient-reported outcome measures in people with knee osteoarthritis.
5. Lack of Physical Activity
- Cause: Inactivity weakens muscles that support the joint, worsening stiffness.
- Fix: Low-impact movement is your friend. Swimming, tai chi, or cycling maintain flexibility without overloading the joints.
The idea of resting too much might sound comforting, but it’s actually one of the biggest traps. Muscles weaken, joints stiffen, and inflammation builds in the background.
Gentle daily movement keeps synovial fluid circulating — which is key for nourishing joint cartilage and maintaining range of motion.
6. Injury or Joint Trauma
- Cause: Old injuries or new sprains can trigger OA flare-ups due to tissue stress.
- Fix: Seek musculoskeletal care; MRI scans or joint fluid analysis may guide therapy. Use braces or supportive devices if needed during healing.
Even an old ankle sprain or minor fall can wake up dormant inflammation. Your body “remembers” trauma, especially in degenerative joint disease.
Working with orthopedic specialists can help identify weak points through imaging or joint aspiration and design a personalized recovery plan.
7. Hormonal Fluctuations (especially in women)
- Cause: Changes in estrogen can heighten joint inflammation.
- Fix: Track symptom timing. Ensure balanced nutrition and consider consulting a Summit provider or endocrinologist if cycles strongly affect flares.
Estrogen helps protect joint cartilage, so when levels drop — like during perimenopause — inflammation can creep up. It’s subtle but noticeable.
Adding more anti-inflammatory foods and staying consistent with gentle exercise can balance hormones and support OA flare duration reduction.
8. Cold or Damp Weather
- Cause: Reduced circulation and muscle tightness.
- Fix: Layer clothing, stretch before bed, and use warm compresses during flare season.
Cold air makes muscles tense and restricts blood flow to already inflamed joints. You might even feel your cervical spine stiffen after a chilly walk.
Try layering with soft thermal wear, or warm up with light movement — a 10-minute stretch routine helps maintain joint flexibility through winter.
9. Medication Side Effects
- Cause: Some anti-inflammatory medicines or steroids can paradoxically alter immune response.
- Fix: Discuss with your doctor; they might switch to gentler targeted therapies or adjust dosage. Refer to NPS MedicineWise or the Targeted Therapies Alliance for trusted medication guidance.
Certain medications that help short-term may quietly worsen symptoms later, especially after corticosteroid injections or long-term NSAID use.
Keeping open communication with your rheumatology team ensures you’re balancing relief with long-term arthritis care safety.
10. Posture or Biomechanical Stress
- Cause: Poor alignment adds strain to joint bone spine areas, especially in the cervical spine or knees.
- Fix: Use ergonomic tools, maintain neutral posture, and strengthen surrounding muscles with a specialist’s guidance.
Small posture tweaks — like how you sit or stand — can make a huge difference. Misalignment quietly stresses the joint’s cartilage, speeding up wear and tear.
A simple ergonomic chair, supportive shoes, or guidance from the Accessible Design Division can drastically reduce future OA flare-ups.
III. Symptoms: How to Know You’re Having a Flare-Up
It’s tricky sometimes — wondering if today’s stiffness is just another “normal” OA day, or if a true osteoarthritis flare-up is kicking in. You might feel it before you can name it: that dull ache turning sharp, your knee suddenly heavier, movement slower.
A flare-up usually has a distinct rhythm — more intense pain, deeper fatigue, and a kind of unspoken frustration that creeps in.
The first clue? Pain intensity. Your usual background ache shifts into something more insistent — sharper, longer lasting, and less responsive to your go-to remedies.
A. Pain and Tenderness Patterns
In a joint flare, pain often localizes around one or two joints, especially those under constant use — knees, hips, or hands. The ache deepens with pressure or after long periods of standing.
It’s a mix of stiffness, burning, and tenderness, reflecting heightened nerve sensitivity and inflammatory markers at play.
Even touching the joint can sometimes feel uncomfortable — your body’s way of signaling that synovial inflammation is active again. People often describe the sensation as “a bruise beneath the skin” or “a bone-deep ache that won’t let up.”
B. Swelling and Warmth in Joints

When the joint’s cartilage becomes irritated, your body floods the area with synovial fluid to cushion the impact. That’s why joints may look puffy or feel warm to the touch. It’s the inflammation doing its job — just a bit too enthusiastically.
Warm compresses and light massage may help ease that tight, full feeling. Doctors sometimes confirm inflammation through joint fluid analysis or MRI scans if it persists.
Pro Tip: If one knee or hand swells but the other doesn’t, it’s probably mechanical OA inflammation — not autoimmune childhood arthritis or rheumatoid arthritis, which usually affects joints symmetrically.
C. Stiffness After Rest or Activity

Another hallmark symptom is stiffness — that frustrating “cement joint” feeling after sitting too long or waking up. Unlike inflammatory arthritis, OA stiffness tends to improve as you move. Gentle stretching or heat packs can speed that up.
If stiffness worsens as the day goes on, it might mean your joints are overloaded. That’s your signal to scale back activity — not stop moving, but adjust your pace.
D. Emotional and Sleep Disruption
Pain isn’t just physical; it leaks into everything — your mood, your patience, even how well you sleep. Many people in pain trajectory groups report higher anxiety or mild depression during long flares.
Poor sleep fuels inflammation further, creating a feedback loop. It helps to treat rest like therapy — a priority, not a luxury. Mindfulness or short-form McGill Pain Questionnaire (SF-MPQ-2) guided exercises can help reduce the brain’s hyper-awareness of pain.
IV. How to Treat Osteoarthritis Flare-Ups (Evidence-Based & Natural Options)
When a flare hits, your first instinct might be to stop everything — rest, hide under a blanket, and wait it out. But treatment isn’t just about relief; it’s about helping your joints recover smarter. Effective care blends medical, physical, and even psychological support — because osteoarthritis is as much about how you live as what you treat.
A. Medical Treatments
For moderate to severe flare-ups, anti-inflammatory medicines remain the go-to option. NSAIDs like ibuprofen or naproxen can reduce inflammation and improve range of motion. When pain becomes more stubborn, doctors might use corticosteroid injections or cortisone injections to calm inflammation quickly.
In some cases, joint aspiration can relieve pressure from excess fluid. If flares become frequent, your rheumatology team might suggest long-term strategies like targeted therapies or joint replacement surgery for advanced knee osteoarthritis.
Medical Approaches to Flare Relief
| Treatment | Purpose | Typical Use | Notes |
| NSAIDs | Reduce pain & swelling | Mild to moderate flares | Monitor stomach irritation |
| Corticosteroid Injections | Quick inflammation control | Severe or recurring flares | Usually limited to 3–4 times/year |
| Physical Therapy | Improve flexibility & posture | During recovery | Aids degenerative joint disease progression control |
| Joint Aspiration | Relieve pressure & confirm cause | If swelling persists | Often used in diagnostic settings |
Pro Tip: Always discuss flare frequency with your doctor. Frequent injections or overuse of pain meds may mask deeper issues like cartilage breakdown or bone spurs that need imaging or structural treatment.
B. Home Remedies
Sometimes, the simplest comforts do the most good. A warm compress in the morning, a cool pack after long walks, or Epsom salt baths can all soothe the ache. Alternating heat and cold therapy helps maintain steady circulation and prevents joint stiffness.
Try pairing these with gentle stretching or massage — nothing aggressive, just light movement to remind your joints they’re still capable. Many patients in arthritis care research studies found consistent self-care reduced OA flare duration by nearly 30%.
Herbal balms with turmeric, capsaicin, or ginger also show mild benefits. They’re not miracle cures, but they help — and sometimes, feeling like you’re doing something helps even more.
C. Natural & Holistic Approaches
A growing number of specialists (including teams from University of Liverpool and Versus Arthritis) now promote holistic approaches alongside medication. Diet, supplements, and mind-body methods can significantly shape your pain experience.
- Supplements: Glucosamine, chondroitin, and vitamin D support joint cartilage resilience.
- Omega-3 fatty acids: Naturally reduce inflammatory cytokines, improving joint fluid quality.
- Collagen peptides: Help rebuild soft tissue structure around the joints.
There’s also emerging interest in immune-regulating factors like Treg cell support through diet and moderate exercise — showing how lifestyle subtly controls inflammatory markers.
D. Mind-Body Techniques
You can’t fully separate joint pain from mindset, Mindfulness, meditation, and controlled breathing — yes, they actually work. The brain’s pain perception changes with these practices, which is why patient-reported outcome measures often improve even without major medication shifts.
A few minutes of breathwork daily can reduce flare anxiety. Pair that with soft music, sunlight, or journaling about your pain triggers, and you’ll start seeing connections — patterns that make management more predictable.
Pro Tip: Apps like Calm or Insight Timer have arthritis-specific meditations. They don’t cure flares, but they help quiet that fight-or-flight tension that worsens pain cycles.
V. Exercise During an Osteoarthritis Flare-Up: Move Smarter, Not Harder

When your joints feel like they’re fighting you, moving can sound like the last thing you want. But oddly enough, gentle exercise during an osteoarthritis flare-up often makes recovery faster and less painful. It’s not about intensity — it’s about movement quality and awareness.
Regular activity improves blood flow to your joint cartilage, keeps your synovial fluid circulating, and maintains flexibility. But when pain spikes, you have to adjust — not quit.
A. Low-Impact Movement Ideas
Instead of skipping all physical activity, focus on joint-friendly workouts that reduce load while maintaining mobility.
Best Exercises During a Flare-Up
| Type | Example | Benefit |
| Range of Motion | Slow knee bends, wrist rolls | Keeps stiffness away |
| Water Aerobics | Swimming or walking in a pool | Buoyancy reduces joint stress |
| Yoga & Tai Chi | Gentle poses, deep breathing | Improves balance and pain tolerance |
| Resistance Bands | Light tension workouts | Strengthens stabilizing muscles |
You can still “train” even when your joints are cranky — just trade high impact for slow resistance. These moves support your ligaments and cartilage instead of compressing them.
Pro Tip: If you feel warmth, not pain, after exercise — you’re doing it right. If pain lasts more than 2 hours afterward, it’s your body’s cue to rest.
B. How to Pace Your Activity
The key is listening — not to your playlist, but your body’s whispering limits. Flare-ups aren’t the time for new challenges or pushing through sharp pain. But mild discomfort is okay; it’s your body re-learning safe motion patterns.
Try the 10-2-10 rule:
- Move for 10 minutes, rest for 2 minutes, and repeat up to 3–4 cycles.
This structure keeps inflammation in check while still feeding your joints the movement they need to heal.
Pro Tip: Track your flare-up triggers in a journal. Sometimes pain isn’t from movement but from overuse, dehydration, or even stress. Identifying these helps you modify exercise patterns intelligently.
C. Gentle Strength Building
The best long-term arthritis relief comes from strong muscles supporting weaker joints. But skip heavy gym sessions — focus instead on slow, bodyweight-based routines.
- Wall sits for knees
- Seated leg lifts
- Hand grip exercises for fingers
These micro-movements build stability, reduce the impact on cartilage, and slow degenerative joint disease progression.
Even on bad days, 5 minutes of mindful stretching can help your brain and body reconnect. It’s movement medicine — just quieter.
VI. Diet & Nutrition: The Anti-Inflammatory Plate for OA Relief

Food is one of your most underrated tools for managing osteoarthritis flare-ups. The right meals can ease inflammation, protect cartilage, and even improve your energy on flare-heavy days. Think of your diet as daily therapy for your joints — gentle, consistent, and restorative.
A. What to Eat During and After a Flare-Up
When pain hits, inflammation levels rise — so your diet should calm, not fuel, that process.
Anti-Inflammatory Foods That Support Joint Health:
| Food Type | Example | Benefit |
| Fatty Fish | Salmon, sardines, mackerel | Rich in omega-3s, reduce joint swelling |
| Fruits & Veggies | Berries, spinach, kale | High in antioxidants & polyphenols |
| Whole Grains | Quinoa, oats, brown rice | Support gut health & reduce inflammation |
| Nuts & Seeds | Chia, flaxseed, walnuts | Contain ALA (plant omega-3s) |
| Spices | Turmeric, ginger, garlic | Block inflammatory pathways (COX-2 inhibition) |
Even small dietary swaps — olive oil instead of butter, herbal tea instead of soda — can shift your body’s inflammation threshold.
Pro Tip: Add turmeric to your morning smoothie. Combined with black pepper (piperine), it boosts absorption by 2000%, helping ease stiffness faster.
B. Foods to Avoid During OA Flares
Some foods may subtly worsen inflammation and pain. Limiting them can make your flare duration shorter and recovery smoother.
Common Trigger Foods for Arthritis Flares:
- Processed snacks are high in refined sugar
- Fried foods with trans fats
- Red and processed meats
- Drink Excessive alcohol or sugary sodas
- White bread and pasta (high glycemic index)
Cutting these doesn’t mean cutting flavor — experiment with Mediterranean-style meals rich in herbs, olive oil, and fresh vegetables. This approach consistently scores high in studies for joint inflammation reduction.
C. Supplements Worth Considering
When diet alone can’t meet nutrient needs, certain supplements can help:
- Glucosamine & Chondroitin: Support cartilage elasticity
- Vitamin D3: Crucial for bone and joint strength
- Collagen peptides: Assist in joint tissue repair
- Boswellia Serrata: Ancient anti-inflammatory herb shown to reduce OA symptoms
Pro Tip: Always introduce one supplement at a time. That way, you’ll know what’s actually helping your joint pain relief and what’s just hype.
VII. Prevention: How to Reduce Future Flare-Ups
Once you’ve been through a few osteoarthritis flare-ups, you start noticing a pattern — or at least, you think you do. Maybe it’s after a long drive, a few nights of poor sleep, or when the weather changes and your knees ache before the rain hits. Managing a chronic condition like osteoarthritis isn’t just about reacting — it’s about anticipating.
Flare prevention is a mix of science and self-awareness. It’s less about strict rules and more about habits that stack up quietly over time — the kind that keep your joint pain from dictating your week.
A. Keep Moving, But Gently
Movement isn’t optional — it’s your body’s lubrication system. When you move, synovial fluid flows and nourishes your cartilage, helping prevent stiffness.
- Try short daily walks or gentle stretching routines.
- Focus on range-of-motion exercises for knees, hips, and wrists.
- Avoid long sedentary periods — even standing up every hour counts.
Pro Tip: Use a joint-friendly timer method — 25 minutes sitting, 5 minutes stretching. This small rhythm helps reduce the risk of joint stiffness and micro-inflammation that can lead to a flare.
B. Maintain a Healthy Weight
Extra pounds mean extra stress — especially on load-bearing joints like the knees and hips. Even a small weight loss (around 5–10%) can dramatically improve knee osteoarthritis symptoms and lower OA flare frequency.
Quick Guide:
| Goal | Benefit |
| Weight reduction by 5–10% | Lowers knee joint load |
| Balanced BMI | Improves range of motion |
| Anti-inflammatory diet | Reduces systemic inflammation |
It’s not just about aesthetics — it’s about physics. Less load = less wear on the joint’s cartilage.
C. Manage Stress Like It’s Medicine
Believe it or not, stress is a common OA trigger. Cortisol and inflammation tend to rise together, which can worsen pain perception and flare intensity.
- Practice mindfulness or short breathing sessions daily.
- Yoga, tai chi, or journaling can lower inflammatory markers.
- Don’t underestimate the impact of emotional well-being on physical pain.
Sometimes your joints aren’t just stiff — they’re trying to tell you that your nervous system needs rest too.
D. Track and Understand Your Patterns
Keep a simple flare journal or use a phone app to log pain levels, weather, diet, and activity. Over time, you’ll see patterns emerge — maybe certain foods or sleep habits correlate with pain spikes.
Pro Tip: Use a 1–10 pain scale like the Short-Form McGill Pain Questionnaire (SF-MPQ-2) to monitor symptoms consistently. Pairing data with reflection helps your rheumatology team or orthopedic specialist personalize your care.
E. Regular Check-Ins With Professionals
Even if your osteoarthritis symptoms feel manageable, periodic assessments help detect early joint damage or cartilage breakdown.
- Schedule annual MRI scans or joint fluid analysis if recommended.
- A rheumatologist, occupational therapist, or orthopedic surgeon can assess flare trends.
- Clinics like the Cleveland Clinic, Access Ortho, or Versus Arthritis often provide updated care protocols or supportive devices.
Prevention isn’t perfection — it’s small steps that keep pain manageable and predictable.
VIII. When to See a Doctor
Sometimes an osteoarthritis flare-up isn’t just a passing episode — it’s a signal. Knowing when to call your doctor (or seek urgent care) is key to preventing long-term joint damage or complications.
A. Warning Signs That Deserve Attention
If your pain goes beyond your usual pattern — or lasts longer than 2–3 weeks — it might be time to consult your rheumatology team.
Seek medical evaluation if you notice:
- Swelling that doesn’t subside after rest
- Redness or warmth around joints (possible infection)
- Fever or unexplained fatigue
- Locking, grinding, or severe stiffness in the cervical spine or knees
- Rapid increase in pain intensity after corticosteroid injections
Pro Tip: Keep a quick-reference symptom chart. Sometimes, what feels like a typical OA flare might be an overlapping condition like rheumatoid arthritis or psoriatic arthritis, especially if multiple joints swell at once.
B. Diagnostic Steps Your Doctor May Take
A healthcare provider might perform several tests to pinpoint what’s going on:
- Blood tests to check inflammatory markers (CRP, ESR).
- Joint aspiration (fluid removal) for infection or autoimmune arthritis screening.
- X-rays or MRI scans for cartilage and bone changes.
- Patient-reported outcome measures to assess how pain impacts daily function.
This data helps differentiate between a temporary OA pain exacerbation and progression toward degenerative joint disease.
C. Getting the Right Support
Once diagnosed, your provider might refer you to a summit specialist or musculoskeletal care program for a personalized plan.
- Physical therapy to rebuild strength safely.
- Occupational therapy to improve daily function.
- Targeted Therapies Alliance resources for advanced or persistent flares.
Your arthritis care team can tailor treatment — from corticosteroid injections to mobility devices — based on your flare frequency, lifestyle, and emotional health.
D. When Emergency Care Is Needed
Rarely, an OA flare can mask something serious like an infection or a fracture.
Call for urgent care if:
- You can’t move a joint suddenly.
- Pain is sharp and unrelenting.
- There’s visible deformity or fever.
Pro Tip: It’s always better to over-report than underplay your pain. Early intervention prevents joint replacement surgery and preserves function.
Seeing a doctor isn’t just about fixing a flare — it’s about safeguarding your future movement. You deserve to walk, stretch, and rest without constant uncertainty.
IX. Mental & Emotional Well-Being During Flare-Ups
Let’s be honest — sometimes, it’s not the pain itself that breaks you down, but the constancy of it. The quiet, lingering ache that seeps into your routine, your sleep, your patience.
Living with osteoarthritis flare-ups means learning to ride waves you can’t always predict. And that unpredictability… it messes with your head.
You’re not just managing joint pain — you’re managing frustration, fatigue, and fear of the next flare. This is where emotional care becomes as important as physical therapy.
A. Understanding the Mind–Body Connection
Studies in Osteoarthritis & Cartilage and Arthritis Care & Research journals show that pain intensity isn’t purely physical — it’s amplified by psychological stress. Anxiety and depression can heighten pain perception, while chronic inflammation can, in turn, worsen mood.
So yes — it’s all connected.
Pro Tip: Don’t dismiss your emotions as “mental.” Your nervous system processes pain and emotion through overlapping neural pathways. So calming your mind literally helps calm your joints.
B. Small, Honest Coping Strategies
You don’t have to become a meditation master overnight. Sometimes, emotional well-being starts with small, forgiving acts of self-care:
- Five-minute mindfulness breaks: Close your eyes and breathe — deeply.
- Community support: Local arthritis circles or forums like Versus Arthritis help you feel less isolated.
- Gentle journaling: Track emotions alongside symptoms — you might notice patterns between stress spikes and flare severity.
- Talk therapy: Cognitive behavioral therapy (CBT) helps many patients reframe pain responses.
And honestly? Some days you’ll still feel discouraged. That’s okay. Healing doesn’t have to look graceful.
C. Balancing Independence and Support
As flare-ups stretch your patience, it’s tempting to withdraw. But leaning on others — a rheumatology nurse, occupational therapist, or even a friend who just listens — can lighten your emotional load.
Pro Tip: Ask your provider about accessible design devices like jar openers or ergonomic keyboards. Sometimes reducing the strain on your joints reduces the mental burden too.
Quick Reflection Table:
| Challenge | Emotional Impact | Support Option |
| Nighttime pain | Sleep disruption, irritability | Warm compress + magnesium tea |
| Reduced mobility | Loss of independence | Adaptive tools, home adjustments |
| Flare unpredictability | Anxiety, fear of activity | Journaling & therapy check-ins |
| Chronic fatigue | Hopelessness | Light exercise + CBT sessions |
There’s a quiet strength in acknowledging your limits — and then still showing up for your own care.
Conclsuion
So, how long do osteoarthritis flare-ups last? The truth is, there’s no universal timeline — some flare-ups fade in a few days, while others may stretch into weeks. Over time, as you learn your body’s rhythms, these episodes become more predictable and manageable.
You start to recognize triggers — maybe cold weather stiffens your joints or missing your anti-inflammatory meals makes mornings tougher. Awareness becomes your most valuable tool, helping you catch early signs and take action before pain intensifies.
Living with osteoarthritis means learning to balance movement, rest, and mindful care. It’s not just about managing symptoms but about living with intention and gentleness toward your body.
Regular exercise, an anti-inflammatory diet, and staying connected with your healthcare team can all reduce the duration and severity of flare-ups. Over time, you build confidence — knowing that each flare is temporary and that you have the tools to navigate it with less stress and more control.
Ultimately, how long do osteoarthritis flare-ups last depends as much on external factors as on how you respond to them. With the right mindset and self-care habits, you can shorten their duration, reduce their impact, and reclaim comfort and joy in daily life. Progress may not always be linear, but every small step — every gentle stretch and balanced meal — brings you closer to steadier, more resilient living.
People Also Ask
1. What is the best way to manage osteoarthritis?
The best way to manage osteoarthritis is through a mix of low-impact exercise, weight control, an anti-inflammatory diet, and prescribed medications. Consistency and joint-friendly habits are key. Regular monitoring with your doctor helps track progress and adjust treatment early.
2. What exercise is good for osteoarthritis?
Low-impact exercises like swimming, cycling, yoga, and walking help maintain flexibility and strengthen joints without adding stress or pain. Gentle stretching before and after workouts can further prevent stiffness.
3. How do you stop osteoarthritis from progressing?
You can slow progression by staying active, maintaining a healthy weight, managing inflammation, and following your doctor’s treatment plan. Early lifestyle changes can protect cartilage and preserve mobility.
4. What should you not do with osteoarthritis?
Avoid high-impact activities like running on hard surfaces, heavy lifting, or ignoring pain signals — they can worsen joint damage over time. Overexertion and poor posture can also increase strain on affected joints.
5. What is the biggest cause of osteoarthritis?
The main cause is joint wear and tear from aging, but factors like obesity, injury, genetics, and repetitive strain can accelerate it. Overuse without proper rest or recovery also contributes significantly.
6. What is the best vitamin for osteoarthritis?
Vitamins D, C, and K are essential — they support bone strength, collagen formation, and cartilage health for better joint function. Adding omega-3 fatty acids and calcium can further enhance joint protection.
7. What age does osteoarthritis start?
Osteoarthritis often begins after age 40, though earlier onset can occur from injury, genetics, or lifestyle factors. Preventive care in your 30s can delay its onset and reduce long-term severity.
8. What is the best diet for osteoarthritis?
A Mediterranean-style diet rich in fruits, vegetables, omega-3 fats, and whole grains helps fight inflammation and support joint health. Limiting processed foods and sugar can further reduce pain and swelling.
9. Can walking improve osteoarthritis?
Yes, walking strengthens muscles, increases flexibility, and lubricates joints, reducing stiffness and long-term pain. It’s one of the safest, most effective daily movements for joint health.
10. Is the sun good for osteoarthritis?
Moderate sun exposure boosts vitamin D levels, which supports bone and joint health — just be mindful of overexposure. Aim for short, safe doses of sunlight several times a week for best results.



