Just found out you have periodontitis and wondering, Is periodontitis reversible? Yeah, that word sounds intense but before you panic let’s talk about what it means. Is this just one of those scary dentist words meant to push deep cleanings and appointments you don’t want? Or… is periodontitis really something serious?
Honestly, yeah—it’s a big deal. But not always in the way people think. So, is periodontitis reversible? Periodontitis isn’t a death sentence for your teeth removal, but it is your mouth’s way of screaming for help. Early stages? You’ve got a shot at reversing the damage.
More advanced? It gets tricky—but not hopeless. This isn’t about doom and gloom. It’s about learning what’s really going on with your gums, what’s still possible, and what kind of changes might genuinely turn things around.
Whether you’re noticing bad breath, bleeding gums, or your dentist just dropped the “scaling and root planing” bomb, it’s okay to feel a bit overwhelmed. But asking yourself is periodontitis reversible is actually a good place to start. Let’s slow it down and take this one step at a time. You might be surprised how much you can still control.
✅ What Does It Mean to Have Periodontitis?

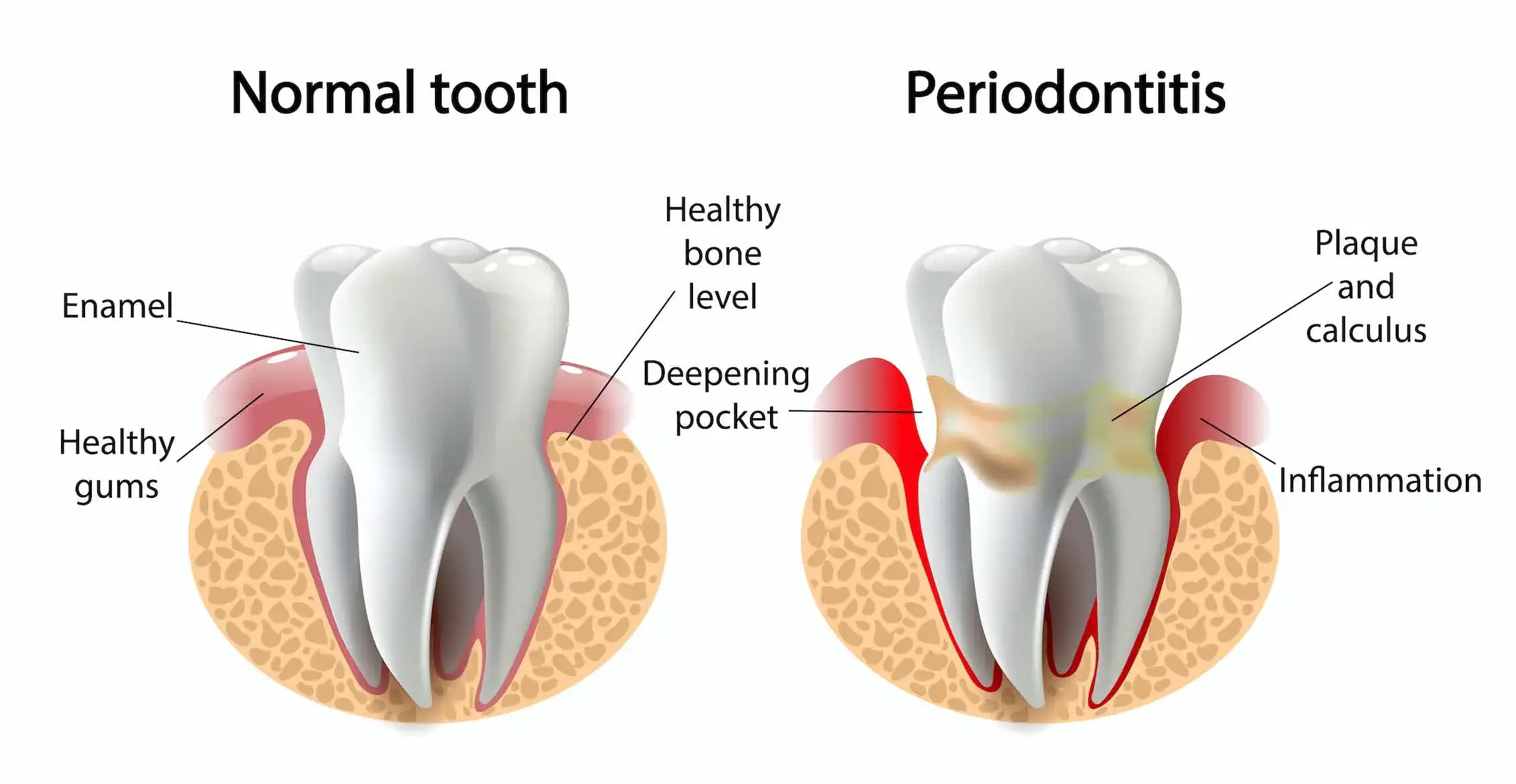
Periodontitis is a step beyond just slacking on flossing or forgetting your dental checkups. It starts quietly—maybe with a little redness or gingivitis, that early inflammation of the gums. But if plaque and tartar buildup aren’t cleared away, bacteria dig deep. And by the time it’s officially “periodontitis,” things have already progressed beneath the surface making people wonder, is periodontitis reversible at this stage?
The Stages of Periodontal Disease

Here’s a quick breakdown of how it typically unfolds:
| Stage | What’s Happening | Common Signs |
| Gingivitis | Gum inflammation, no bone loss yet | Bleeding when brushing, mild irritation |
| Early Periodontitis | Bone begins to break down | Gum sensitivity, mild recession |
| Moderate Periodontitis | Gum pockets deepen, and more bone damage | Halitosis, loose teeth, visible gum pulling back |
| Advanced Periodontitis | Severe bone loss, possible tooth loss | Teeth shifting, chronic bad breath, and pain chewing |
At this point, the gums may detach from the tooth roots, creating gum pockets where more bacteria collect. Not great. But here’s the thing: while the advanced stage might not be fully reversible, early to moderate cases? There’s still hope.
So, can all stages of periodontitis be reversed? Unfortunately, no. But many cases can be halted and even partly healed—if caught early and treated seriously. The deeper the damage (especially to the bone), the more it shifts from “reversible” to “manageable.”
1. Is Periodontitis Reversible at Any Stage?

It’s probably the first thing on your mind: “Is it too late for me?” Let’s clear that up.
Early vs. Advanced Cases — What’s Treatable?
In the early stages, when inflammation hasn’t yet caused deep bone loss, the answer is: yes, it’s very likely reversible. With consistent oral hygiene, proper brushing, and maybe a round of scaling and root planing, the gum tissue can reattach, inflammation reduces, and you might even dodge further progression altogether.
But once the disease has moved deeper—if bone degradation is visible on dental X-rays, or if your gums have pulled far away from the gumline—things get more complicated. In these cases, treatment can stop things from getting worse, but can it reverse all the damage? That’s a long shot. The term shifts from “cure” to “control.”
When It’s Too Late for Full Reversal
Once you’ve got deep gum recession, exposed roots, or mobile teeth hurt due to bone loss, it’s unlikely your mouth can just bounce back without more advanced help, like gum grafts, bone grafting, or periodontal surgery. And even then, it’s more like rebuilding a house with missing bricks than pressing “undo.”
According to the American Academy of Periodontology, early intervention and consistent maintenance are critical. And while you can’t regrow bone naturally, there are techniques like Guided Tissue Regeneration that can help rebuild what was lost, to some extent.
But don’t panic. If you’re somewhere in the middle, there’s still a solid chance to stop things in their tracks and avoid more dramatic procedures.
2. How Deep Cleaning Can Help Reverse Gum Damage

Early periodontitis is reversible with consistent care. If you’re asking is periodontitis reversible, the answer is yes, especially in the early stages. Since bone isn’t yet affected, non-surgical treatments, improved hygiene, quitting smoking, and regular dental cleanings can halt progression and restore gum health before it worsens.
What Is Scaling and Root Planing?
Scaling and root planing (SRP) is like a reboot for your gums. It’s not just a fancier cleaning—it goes below the gum line, targeting the tartar, plaque buildup, and bacteria that your toothbrush and floss can’t touch.
| Term | What It Does |
| Scaling | Removes hardened calculus and plaque from teeth and under the gums |
| Root Planing | Smooths the tooth roots so the gum tissue can reattach and heal |
This process reduces inflammation, shrinks gum pockets, and gives your gums a clean slate to start recovering. For early to moderate periodontal disease, this treatment alone—paired with strong aftercare—can reverse the inflammation and help the gums heal.
Now, if your case is advanced periodontitis, SRP might not reverse all the damage, but it can absolutely prevent further bone loss and create the foundation for more specialized treatments like laser therapy or gum grafts later on.
Does It Hurt? How Long Is the Recovery?
Okay, honesty time: yes, scaling and root planing can be a little uncomfortable, especially if your gums are already tender. Most dentists offer dental sedation, topical anesthetics, or local numbing to make it manageable. You might feel soreness for a day or two, maybe a little gum recession if the inflammation shrinks.
Recovery tip: Stick with soft foods, use a prescribed antimicrobial mouthwash, and avoid smoking or alcohol for at least 24–48 hours. This is your gums’ recovery window—don’t mess with it.
Pro Tip: Ask your dental provider if they use tools like the Cavitron Touch or ultrasonic scaling systems. These newer technologies are more comfortable and may reduce post-treatment soreness compared to traditional tools.
3. At-Home Habits That Can Make (or Break) Your Progress
Let’s not sugarcoat it: even the best dental treatments can fail if you go home and treat your teeth like a suggestion box. Daily habits—especially your oral hygiene routine—can either support your healing or quietly sabotage it.
Proper Brushing and Flossing for Gum Health

Start with the basics, but upgrade your game. Your old brushing routine? Probably not cutting it anymore.
Here’s what an ideal gum-friendly routine looks like:
- Brush twice daily with a fluoride toothpaste (ADA-approved)
- Use a soft-bristled toothbrush or, even better, an electric toothbrush for consistent pressure and motion
- Floss once daily to break up food particles and bacteria
- Consider dental picks or interdental brushes if your gums are sensitive
- Follow up with an anti-bacterial mouthwash (especially one with chlorhexidine if prescribed)
Pro Tip: Switch to an electric toothbrush with a pressure sensor if you tend to brush too hard—aggressive brushing can worsen gum recession and delay healing.
Mouthwashes and Water Flossers – Which Ones Work?

While mouthwash isn’t a magic solution, certain types really do help with plaque control and bacterial reduction, especially during healing from deep cleaning procedures.
| Product | Purpose | Best For |
| Antimicrobial mouthwash | Reduces bacteria in gum pockets | Post-scaling recovery |
| Fluoride rinse | Strengthens enamel | Those with early tooth decay risk |
| Water flosser | Gently cleans between teeth and below the gumline | Sensitive gums or post-treatment care |
If you’ve got deep pockets or ongoing inflammation, a water flosser can help flush out areas that traditional floss misses. Just make sure you’re using it daily, not once a week when you remember.
And yep, using these tools consistently? It might honestly be more important than anything your dental team does. What you do between appointments can decide whether your gums fully recover, or quietly slip back into trouble.
4. Diet and Nutrition for Gum Healing

Your gums eat what you eat. Not literally, of course—but if you’re asking, is periodontitis reversible? Your diet plays a surprisingly big role in that answer.
The connection between food and oral health is more than just avoiding sugar. Certain foods promote tissue repair, reduce inflammation, and support the immune system’s ability to fight off the bacteria lurking around your gumline. Others… do the exact opposite.
Anti-Inflammatory Foods for Oral Health
To encourage healing in your gum tissue (and possibly support mild reversal of periodontal disease), try loading your plate with:
- Leafy greens like spinach and kale are packed with vitamins A and C
- Fatty fish (salmon, sardines) – rich in omega-3s that help reduce inflammation
- Citrus fruits (in moderation) – for collagen production and vitamin C
- Green tea – natural antioxidant and antimicrobial properties
- Nuts and seeds – zinc and vitamin E help regenerate tissue
- Low-fat dairy – calcium to support the bone structure beneath your teeth
Avoiding refined sugars, acidic sodas, and overly processed carbs can also help prevent plaque buildup and reduce the fuel that bad oral bacteria thrive on.
Here’s a quick reference:
| Meal or Snack | Gum-Friendly Reason |
| Greek yogurt with flaxseeds | Calcium + omega-3 combo |
| Raw carrots and hummus | Crunchy, plaque-clearing fiber |
| Boiled eggs with avocado | Protein + healthy fat = healing support |
| Berries with green tea | Anti-inflammatory antioxidant power |
| Tuna sandwich on whole grain | Omega-3s + vitamin B12 |
Pro Tip: Your gut health affects your oral health more than you might think. Try a probiotic supplement or foods like kimchi and kefir to support a healthier oral microbiome indirectly.
What to Avoid (Sugar, Alcohol, Smoking)
It’s not just about what you eat—it’s also what you ditch. If your oral care routine is solid but your diet is junky, your gums are constantly under attack.
Watch out for:
- Sugary snacks or drinks (fuel for bacteria = worse tartar buildup)
- Alcohol (dries out your mouth, weakening your natural defense system)
- Sticky foods that linger on teeth (even dried fruit can be sneaky)
- Highly acidic drinks like sodas or citrus juices (enamel erosion + inflammation)
And yes… that leads us to the elephant in the room.
5. Does Smoking Stop Your Gums From Healing?

It’s one of the most well-documented truths in periodontal care: if you smoke, your chances of healing go down dramatically. In fact, many periodontists consider smoking a major reason why some patients don’t respond to treatment at all, even if they’re doing everything else right. So if you’re wondering is periodontitis reversible while still smoking, the answer becomes a lot more complicated.
Why Smoking Worsens Gum Disease
Here’s what smoking does to your gums behind the scenes:
- Cuts off blood flow to gum tissues — less oxygen means slower healing
- Masks signs of inflammation — gums don’t bleed as much, making problems hard to detect
- Increases bacterial growth andthe risk of calculus buildup
- Raises the risk of tooth loss, bone loss, and failed gum grafts or implants
So even if you’re asking, is periodontitis reversible, and you’re following every rule in the book, if you’re still lighting up, your gums are constantly working against the odds.
According to data from the Centers for Disease Control and Prevention, smokers are twice as likely to develop periodontal disease compared to non-smokers. That’s a hard stat to ignore.
Tips to Quit and Help Gums Recover
It’s not easy, but if your gums could talk, they’d probably beg you to quit. Here’s a few strategies:
- Try nicotine replacement therapy (patches, gums, lozenges)
- Join a support group or quit-smoking program—online or local
- Ask your dental provider about prescription options like bupropion or varenicline
- Swap the habit with sugar-free gum, herbal tea, or toothpicks
- Set a small goal—just 3 days, then one week, then two…
And yes, once you quit, your body starts healing pretty quickly. Blood flow returns to your gumline, inflammation drops, and your treatments (like scaling & root planing) become a lot more effective.
Pro Tip: Many dental clinics now offer smoking cessation counseling as part of a full dental treatment plan—ask your dental team if they do.
6. Professional Treatments Beyond Deep Cleaning
So… what if deep cleaning alone isn’t enough? Maybe you’ve already done scaling & root planing, but your gums still feel off. Maybe your periodontist mentioned something about grafts or lasers, and your brain kind of shut down.
At this point, you’re not alone in wondering—is periodontitis reversible, even with extra treatments?
Well, kind of. You can’t undo bone loss or erase gum recession like nothing happened—but some treatments can rebuild, regenerate, and help prevent things from sliding further downhill.
Laser Therapy for Periodontitis

Laser treatments—like diode laser therapy or laser gum therapy—are becoming more common in periodontal care. They’re less invasive than traditional surgery, and some patients say they’re way more comfortable.
How it works: Lasers target and remove infected tissue, sterilize the area, and stimulate healing around the tooth roots.
| Laser Option | What It Helps With | Bonus Benefits |
| Diode Laser | Bacterial removal from deep pockets | Minimally invasive, faster healing |
| LANAP (Laser Assisted New Attachment Procedure) | Regeneration of bone and tissue | Often no cutting or sutures needed |
Laser dentistry might not be for everyone (it can be pricey, and not all clinics offer it), but if you’re dealing with advanced periodontitis, it’s worth asking your dental clinic or dental provider about.
Gum Graft Surgery and Bone Regeneration

If your gum line has pulled back significantly—or your teeth look oddly “long,”—gum grafting might be your next move. It’s exactly what it sounds like: borrowing soft tissue (often from your palate) to rebuild the receding gums.
For bone loss, treatments like:
- Guided Tissue Regeneration
- Dental bone grafts
- Platelet-rich plasma therapy
- Osseous surgery
…can encourage your body to regrow bone in the bone socket areas where it’s been lost. These techniques are especially helpful if you’re considering dental implants down the road.
Pro Tip: Always ask if your clinic partners with specialists for full-mouth rehabilitation or advanced periodontal surgery. A team approach can often offer better outcomes than piecemeal fixes.
7. How Long Does It Take to Reverse Periodontitis?
Periodontitis can return quickly without consistent care, especially if you have diabetes ora genetic risk. Stick to flossing, routine cleanings, and watch for early signs like bleeding or gum tenderness to prevent relapse.
Realistic Timelines for Mild vs. Moderate Disease
Let’s break it down honestly:
| Disease Stage | Approx. Healing Timeline | What You Might See |
| Early/Mild Periodontitis | 2–4 weeks post deep cleaning | Reduced bleeding, tighter gums |
| Moderate Periodontitis | 1–3 months with follow-up visits | Gum pockets shrink, breath improves |
| Advanced Periodontitis | 6 months+ with surgery/therapy | Slowed progression, maintained function |
Keep in mind—these are healing milestones, not finish lines. You don’t “graduate” from gum disease. You manage it like a long-term health condition.
What to Expect During Healing?
During the healing process, your dental appointments will feel more like check-ins than emergencies (which is a good thing). You might feel:
- Minor gum tenderness or swelling after treatments
- Bleeding less often during brushing
- Improved oral hygiene routine compliance (because now it matters more than ever)
- Less halitosis (bad breath), especially in the mornings
But there’s also a mental game here. Healing isn’t always linear. Some weeks, your gums look great, then suddenly one spot feels irritated again. That doesn’t mean you’re failing. It just means your oral care needs consistency, not perfection.
Pro Tip: Celebrate small wins. If your periodontal probe shows improvement in even one area at your next visit, that’s real progress. Track your pocket depth reductions like you would steps on a fitness app.
8. Can Periodontitis Come Back? How to Prevent Relapse
Let’s say your gums are finally looking better. You’ve been showing up for dental visits, brushing like a pro, maybe even bought that electric toothbrush with the Bluetooth app (hey, no judgment). But then a few months pass… you slack off a little… and things feel off again.
So, yeah—this is the part nobody really wants to hear.
Even if you’re asking periodontitis is reversible and getting good news, the reality is that periodontal disease doesn’t really “go away” forever. It goes quiet. And if you don’t keep up, it can roar back louder than ever.
Maintenance Therapy and Routine Care
After your main periodontal treatments, your dentist or periodontist might recommend something called periodontal maintenance. It’s not just a fancier word for cleanings—it’s a structured care plan that often includes:
- Professional dental cleanings every 3–4 months
- More frequent periodontal probing to check gum pockets
- Customized oral hygiene routine recommendations
- Targeted therapies like topical antibiotics or antimicrobial mouthwash
The goal? To keep bacteria, tartar, and plaque buildup from getting a foothold again.
Without this maintenance, relapse becomes way more likely, even after successful scaling/root planing or gum surgery.
Pro Tip: Add your cleanings to your calendar like birthdays. The minute you start treating them as optional… that’s when problems sneak back in.
Long-Term Prevention Strategies
Want to know the unsexy secret to long-term gum health? Boring, consistent habits. Nothing flashy—just daily choices that protect all the progress you’ve made.
Here’s what that looks like:
- Stick to brushing and flossing even when your gums feel “fine”
- Avoid tobacco products entirely (no “just one” slip-ups)
- Stay hydrated to support your oral microbiome
- Use fluoride toothpaste and/or antibacterial rinses daily
- Eat fewer acidic or sugary foods—they quietly fuel gum inflammation
- Don’t skip dental checkups, even if nothing hurts
And hey—if you’re ever unsure whether something’s okay for your gums (like switching to a new mouth wash, trying a trendy diet, or skipping a cleaning)… ask your dental team. Prevention is their full-time job.
9. Is Periodontitis Linked to Other Health Problems?

Here’s where things get even more serious— Is periodontitis Reversible. It’s deeply connected to your overall health, and that makes treating it a much bigger deal than just avoiding the dentist’s drill.
When you have chronic gum inflammation, your mouth becomes a launch pad for bacteria and toxins that can spread to other parts of your body. Over time, this contributes to—or worsens—systemic diseases.
Health Conditions Tied to Gum Disease
Research shows strong links between periodontitis and the following health issues:
- Heart disease – Inflammation and oral bacteria can damage blood vessels
- Diabetes – Gum infection makes blood sugar harder to control, and vice versa
- Respiratory conditions – Oral bacteria may be inhaled into the lungs
- Rheumatoid arthritis – Shared inflammatory pathways worsen both conditions
- Pregnancy complications – Severe gum disease increases risk of low birth weight and preterm birth
If you’re dealing with diabetes, heart problems, or chronic immune issues, treating your gum health might improve your general well-being, too.
There’s a two-way street here: poor oral health affects the body, and chronic health conditions make gum disease harder to control. That’s why early, proactive treatment matters—even if you’re only at stage one.
Final Thoughts
Is periodontitis reversible? In many cases, yes—especially if caught early. With good oral hygiene, non-surgical treatments, and regular dental visits, you can reverse mild to moderate gum disease. But if it’s advanced—like deep gum pockets, receding gums, or bone loss—then full reversal isn’t likely.
Instead, the focus shifts to managing the damage and preventing it from getting worse. Ask yourself: Do your gums bleed when brushing? Do your teeth look longer? Bad breath that won’t go away? These are red flags. Don’t ignore them. Healing your gums takes consistent care, a reset in habits, and support from your dental team. But yes—it’s still possible.
Frequently Asked Questions
1. Can brushing alone reverse periodontitis?
Nope—brushing and flossing help, but once periodontitis starts, you’ll need professional help like scaling and root planing or antibiotic therapy to truly reverse it.
2. Is periodontitis reversible without surgery?
Sometimes, yes. If it’s in the early or moderate stage, non-surgical periodontal treatments like deep cleanings and oral antibiotics can help reverse it.
3. Can I reverse periodontitis naturally?
You can support healing naturally—like using antibacterial mouthwash, eating a gum-friendly diet, and improving oral care—but you still need a dentist’s help.
4. How long does it take to reverse periodontitis?
It depends. For mild cases, you might see improvements in 2–4 weeks after deep cleaning for gum disease, but full healing can take months with regular care.
5. Can gum tissue grow back after periodontitis?
Gum tissue doesn’t regrow naturally once it recedes, but with gum regeneration procedures or grafting, you can rebuild some of what was lost.
6. What happens if I ignore chronic periodontitis?
It’ll likely get worse—causing tooth mobility, bone loss, and even tooth loss. And trust me, it won’t go away on its own.
7. Is periodontitis contagious?
Kind of. You can’t “catch” periodontitis like a cold or the flu, but the oral bacteria that cause it can be spread through saliva. That means kissing, sharing utensils, or drinks might pass those bacteria to someone else—especially if their oral hygiene is poor or their immune system is weak.
8. Can children get periodontitis?
Yes, but it’s rare. Kids may develop aggressive forms linked to genetics or poor hygiene. Regular checkups can catch early signs.
9. Does dental insurance cover gum disease treatment?
Most plans cover non-surgical periodontal treatments like scaling and root planing, but coverage for surgery or laser treatment varies—always double-check your policy.
10. Is it ever too late to treat periodontitis?
It’s almost never too late. Even if it can’t be reversed fully, treatment can slow or stop progression and help you keep your teeth longer.