So here’s the thing — a lot of people start antibiotics with this quiet hope that relief will be instant. You swallow that first capsule, sip some water, and… maybe you wait, half-expecting your sore throat or sinus pressure to fade like flipping a switch. But the real question — how long does it take for amoxicillin to work — is trickier than it sounds.
Amoxicillin is one of those broad-spectrum antibiotics that doctors often prescribe, especially for bacterial infections such as earaches, urinary tract infections, or dental infections when pain spikes at the worst possible moment. It’s part of the beta-lactam antibiotic family — the kind that goes after bacterial cell walls like tiny wrecking crews. And while it’s effective (most of the time), the timeline isn’t always predictable.
Understanding how fast it kicks in isn’t just about curiosity, though. It’s about knowing what to expect so you don’t panic if you’re still coughing after day one, or — just as important — so you don’t stop early thinking you’re “cured.” Finishing the prescribed course matters for your health, and honestly, for everyone’s health, because antibiotic resistance is a real, growing problem.
This piece will walk through ten factors that shape the amoxicillin effectiveness timeline — why sometimes you feel better in 48 hours, and other times it drags on longer. Think of it as a guide that blends the science with the everyday “what do I actually notice?” side of things.
How Long Does It Take for Amoxicillin to Work in the Body

Before getting into timelines, it helps to know what’s happening inside you after you swallow that pill.
Mechanism of Action – What It Actually Does
Amoxicillin works by messing with bacterial cell walls. Imagine bacteria trying to build a sturdy little fortress — amoxicillin slips in and weakens the bricks. The bacteria can’t hold themselves together, and your immune system does the final cleanup. That’s the gist.
It’s considered a broad-spectrum antibiotic, meaning it’s useful against a range of bacterial strains, including things like Escherichia coli in urinary tract infections or Streptococcus in strep throat. The Centers for Disease Control and Prevention notes it’s often a first-line treatment because it’s well-studied, available in different oral formulations (chewable tablets, capsules, liquid suspension), and generally tolerated by most people — unless you’ve got a penicillin allergy.
Common Uses – Where You See It Prescribed
Doctors prescribe amoxicillin all the time. Some of the most common conditions include:
- Ear infections (especially in kids, who seem to collect these like souvenirs).
- Strep throat or tonsillitis, when a throat swab confirms it’s bacterial.
- Urinary tract infections (UTIs) are caused by certain bacterial strains.
- Respiratory tract infections, like sinus infection or bacterial pneumonia.
- Dental issues, such as gum disease or a tooth infection, before a root canal.
- Even more specialized cases, like Lyme disease in early stages or Helicobacter pylori infections when paired with other drugs.
Pro Tip: Not all sore throats, earaches, or coughs need antibiotics. Viral infections — colds, the flu — won’t get better faster with amoxicillin, no matter how badly you want them to. That’s where checking in with a healthcare professional (in person or even through virtual urgent care) can save you the guesswork.
And yes, sometimes doctors prescribe amoxicillin/clavulanic acid (known as Augmentin) instead. That’s basically amoxicillin boosted with clavulanic acid, which helps when bacteria have learned resistance tricks.
Typical Timeline – When You May Feel Better
So, if you’re sitting there after swallowing your first amoxicillin capsule, wondering, “Okay, but how long does it take for amoxicillin to work?” — here’s the rough outline most people experience.
First 24 Hours – The Early Phase
Technically, amoxicillin starts working against bacteria pretty quickly after you take it. It’s absorbed into your bloodstream within an hour or so. But — and this is the frustrating part — you usually don’t feel much symptom relief yet. Your bacterial load is still high, and your immune system is just getting a bit of backup.
48–72 Hours – Noticeable Changes
For many infections, this is when things begin to shift. A sore throat might feel less razor-like, the pressure of a sinus infection may ease, or the burning tip of urethra (from a urinary tract infection) could calm down. According to places like the Cleveland Clinic and Mayo Clinic, most patients report some relief within this window.
Full Course Completion – The Real Finish Line
Here’s the catch: even if you feel better after 3 days, that doesn’t mean the infection is gone. The bacterial culture in your body might still have stragglers. Stopping early not only risks the infection roaring back but also contributes to antimicrobial resistance — the whole “superbug” problem public health experts like Dr. Ghinwa Dumyati warn about.
To make it clear, here’s a quick look at the typical recovery rhythm:
| Timeline | What’s Happening Inside You | What You Might Notice |
| 0–24 hours | Drug absorbed, bacteria cell walls disrupted | Usually no big change in symptoms |
| 48–72 hours | Bacterial load decreases, immune response kicks in | Symptoms begin easing (less pain, swelling, or fever) |
| Day 4–7 | Infection continues clearing, body heals | Steady improvement; you may feel “almost normal” |
| After finishing full course | Infection fully treated, relapse risk reduced | Full recovery (if treatment plan followed) |
Pro Tip: If you don’t notice any improvement after 3 days, or if symptoms get worse, it’s time to call your healthcare professional. Sometimes the bacteria are resistant, or maybe it’s not bacterial at all (like with viral infections or digestive complications that mimic infections).
1. Type and Severity of Infection
This is the first big piece of the puzzle. The kind of infection you have — and how severe it is — really shapes how long amoxicillin take to work.
- Milder infections (like uncomplicated strep throat or a small gum infection) often respond faster. You could notice relief in that 48–72-hour sweet spot.
- More stubborn infections — say, a sinus infection that’s been lingering for weeks or a tooth infection with symptomatic irreversible pulpitis — might drag on. Pain may ease, but full resolution takes longer.
- Complicated cases (like bacterial pneumonia or certain strains of Clostridium difficile) may require stronger combinations, longer dosage regimens, or even IV antibiotics in an emergency medicine setting.
Example – Strep Throat vs. Urinary Tract Infection
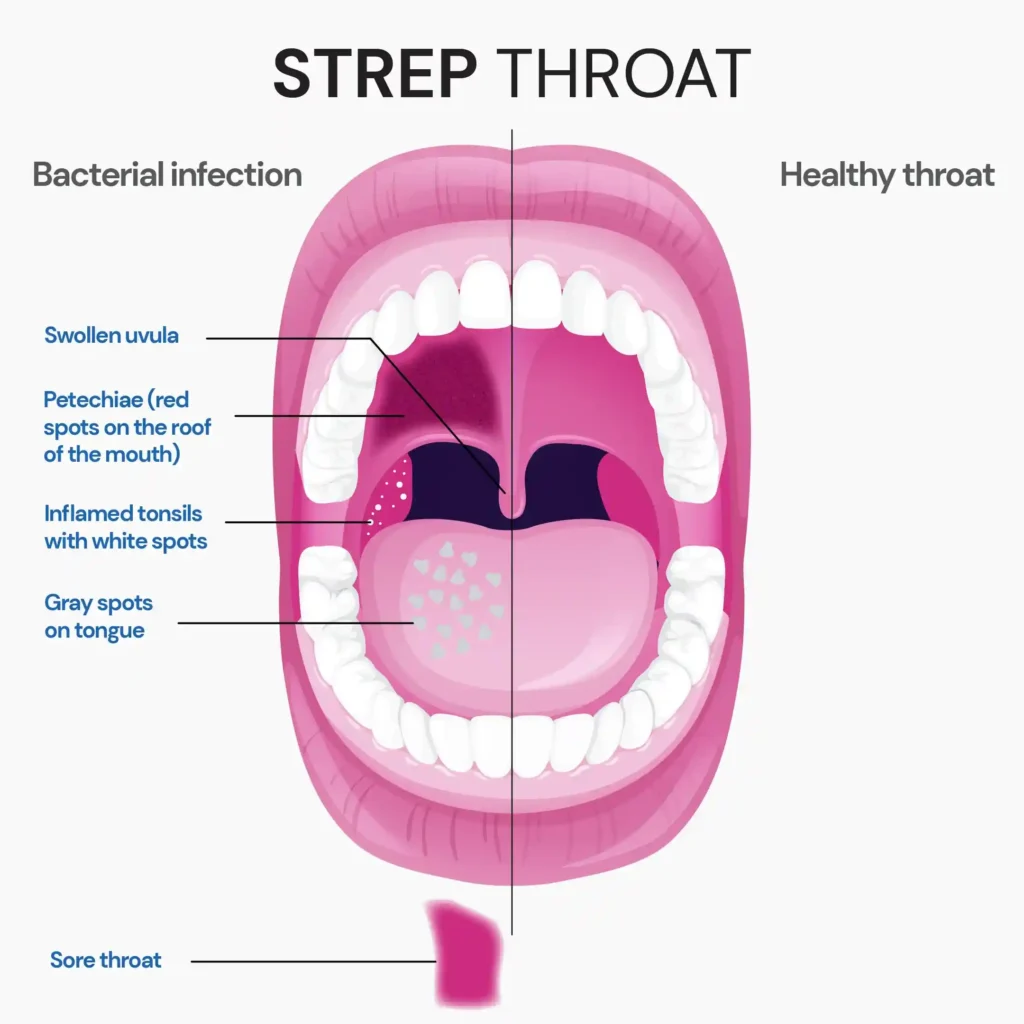
- With strep throat, amoxicillin usually brings noticeable improvement pretty fast (within 2–3 days).
- A urinary tract infection, though, especially if it’s caused by E. coli resistant to standard antibiotic classes, might need more time or even a switch to extended-release tablets or a different medication entirely.
And just to circle back — the severity factor matters too. A mild dental infection caught early is different from a deep-rooted abscess that may eventually need a root canal.
Quick Reminder: If your infection feels worse instead of better after 3–5 days, or you start noticing weird side effects like a rash, digestive complications, or even signs of a yeast infection, don’t just push through. Contact a doctor. Sometimes it’s an allergic reaction, other times it’s amoxicillin resistance at play.
2. Dosage and Frequency
It might sound obvious, but the dose you’re prescribed — and how consistently you take it — has a big influence on how long does it take for amoxicillin to work.
Doctors tailor dosage regimens based on infection type, patient age, and sometimes even body weight. For example:
- Adults: Often 500 mg every 8 hours, or sometimes 875 mg every 12 hours for certain respiratory tract infections.
- Children: Liquid suspension or chewable tablets are more common, with dosing carefully measured in milligrams per kilogram of body weight.
- Serious infections: Extended-release tablets or higher-dose courses may be recommended (like for bacterial pneumonia).
Why Timing Matters
Missing a dose isn’t just a small slip — it actually lowers the steady drug level in your system, giving bacteria a chance to regroup. That’s why medication compliance is such a big deal. Taking two doses at once to “catch up” isn’t ideal either; it risks side effects like nausea or digestive complications without improving effectiveness.
Here’s a quick comparison:
| Dosage Pattern | Likely Outcome | Risk Factor |
| On time, every time | Maximum bacterial clearance | Best results |
| Occasional missed dose | Slower recovery, possible relapse | Antibiotic resistance risk |
| Stopping early | Symptoms may return, stronger bacteria survive | High resistance risk |
| Doubling doses | No faster cure, higher chance of side effects | Digestive upset, yeast infection |
Pro Tip: If you ever miss a dose, most healthcare professionals (and even Mayo Clinic guidelines) say take it as soon as you remember — unless it’s almost time for your next one. In that case, just skip the missed pill.
3. Patient Age and Health Condition

Your age and overall health can quietly influence how fast amoxicillin works.
- Children often metabolize medications differently from adults. That’s why pediatricians are precise with milligram-per-kilogram dosing. Kids with ear infections may bounce back quickly, though sometimes recurrent bacterial strains make things complicated.
- Elderly patients may see slower recovery due to reduced kidney or liver function, which affects how the drug is cleared from the body.
- Chronic health conditions — diabetes, liver disease, and kidney disease — can also delay improvement. Sometimes dosage adjustments are necessary to avoid toxic levels or treatment failure.
Immune System Considerations
It’s not just the drug at work. Your immune system is the other half of the equation. If it’s strong, symptoms may ease faster. But if you’re dealing with immune suppression (from chemotherapy, HIV, or even severe stress), amoxicillin might need more time to tip the balance.
Some doctors — like those at Cleveland Clinic and Pleasant View Dental Clinic — emphasize that amoxicillin’s effectiveness isn’t just about the pill; it’s also about your immune response doing its job alongside it.
Quick Example
- A 25-year-old with strep throat and no underlying issues might feel better in 2 days.
- A 70-year-old with bacterial pneumonia and chronic kidney disease could take longer — maybe 5 days or more before real relief is noticed, even with the same antibiotic classes.
And just to add — people sometimes expect antibiotics to work like painkillers. But the process is more gradual, layered with your body’s healing pace.
4. Bacterial Resistance
Here’s where things get messy. Even if you’re taking your antibiotic exactly as prescribed, sometimes the bacteria just don’t budge. That’s usually a sign of antibiotic resistance — something doctors, pharmacists, and public health experts like those at the Centers for Disease Control and Prevention keep warning us about.
Resistance happens when bacteria evolve ways to dodge the effects of antibiotics like amoxicillin. Some produce enzymes (like beta-lactamase) that literally destroy the drug before it can do its job. That’s why combinations such as amoxicillin/clavulanic acid (better known as Augmentin) were developed — the clavulanic acid helps block those enzymes so amoxicillin can get back to weakening cell walls.
Signs Amoxicillin Might Not Be Working
- No noticeable improvement after 3–5 days.
- Worsening symptoms (like fever climbing higher, cough becoming more severe).
- Infections are coming back quickly after stopping, which could mean the bacteria weren’t fully cleared.
Real-Life Example
Think of a urinary tract infection caused by E. coli. If the strain is resistant, amoxicillin might barely dent it. Doctors might switch to another antibiotic class after reviewing bacterial culture results. This is why labs sometimes run sensitivity tests to figure out which antibiotics will actually work against a specific bacterial strain.
| Infection Type | Amoxicillin Works Well When… | May Fail When… |
| Strep throat | Bacteria are sensitive to penicillin | Early gum disease or a small abscess |
| The bacterial strain is non-resistant | Patient has a penicillin allergy or resistant strain | Resistant E. coli detected in culture |
| Sinus infection | Mild to moderate bacterial load | Chronic sinusitis with resistant strains |
| Dental infection | Patient has a penicillin allergy or a resistant strain | Severe abscess needing root canal |
Pro Tip: If you’re worried about antibiotic-resistant bacteria, don’t stop antibiotics early and don’t pressure doctors for antibiotics when it’s likely viral. That’s part of antimicrobial stewardship — using these drugs responsibly so they keep working when we really need them.
5. Food and Absorption
Okay, so let’s say you’re diligent with your pills. Timing and food still matter. The way your body absorbs amoxicillin can influence how long does it take for amoxicillin to work.
Should You Take It With Food?
Most guidelines say amoxicillin can be taken with or without food. For a lot of people, taking it after a meal actually helps reduce digestive complications like nausea. So no harm there.
But certain foods and drinks can complicate things a little:
- Dairy products: Not as big a deal with amoxicillin as with other antibiotics (like tetracyclines), but still, large amounts of milk or cheese can slightly interfere with absorption.
- Acidic foods/drinks: Things like orange juice or soda may irritate the stomach lining, making side effects like diarrhea or stomach cramps more noticeable.
- Alcohol: Technically doesn’t cancel out amoxicillin’s effect, but it can worsen side effects like dizziness, digestive upset, or even interfere with the immune response.
Food Effects on Amoxicillin
| Food/Drink | Effect on Absorption | Recommendation |
| Dairy (milk, cheese) | Minimal impact, possible stomach upset | Okay in moderation |
| Acidic juices (OJ, soda) | Can increase GI irritation | Take with water instead |
| High-fat meals | Slight delay in absorption | Still effective, but slower onset |
| Alcohol | No direct reduction in antibiotic use | Avoid to reduce side effects |
Pro Tip: If your doctor prescribes extended-release tablets, those should always be taken within an hour of finishing a meal. Otherwise, the absorption pattern gets thrown off, and the effectiveness timeline shifts.
6. Drug Interactions
Sometimes it’s not the infection or even your dosage that slows things down — it’s what else you’re taking alongside amoxicillin. Drug interactions can quietly shape how long does it take for amoxicillin to work.
Common Interactions That Matter
- Birth control pills – Some reports suggest amoxicillin may reduce their effectiveness, though the evidence is debated. Doctors often recommend a backup method, just in case.
- Blood thinners (like warfarin) – Amoxicillin can alter how your body handles these, which means a higher risk of bleeding complications.
- Other antibiotics – Sometimes they’re combined on purpose (like amoxicillin/clavulanic acid), but in other cases, stacking antibiotics from different classes without guidance could cause digestive complications or increase the chance of yeast infection.
- Over-the-counter medication – Even simple antacids or herbal supplements might interfere slightly with absorption.
Here’s a quick table for clarity:
| Medication Type | Possible Effect | What to Do |
| Birth control pills | Reduced effectiveness (controversial) | Use backup protection |
| Blood thinners (warfarin) | Higher bleeding risk | Extra monitoring required |
| Other antibiotics | May help or hinder | Follow specific treatment plan |
| Antacids/herbal meds | Slight absorption changes | Space doses apart |
Pro Tip: Always let your healthcare professional know about everything you’re taking — even vitamins. Something as simple as an iron supplement could affect how amoxicillin capsule absorption works.
7. Immune System Strength
This one doesn’t get talked about enough. The pill itself isn’t doing all the work — your immune system is the real partner in crime here.
If your immune response is strong, you might feel symptom relief sooner. But if it’s weakened — due to chronic illness, chemotherapy, HIV, or even just being run down — then even with antibiotics, the recovery timeline can drag.
Why It Matters
- Healthy immune system → Helps clear the bacterial load faster.
- Weakened immune system → Antibiotics still attack bacteria, but progress may be slower and complications more likely.
- Overactive or misdirected immune response → Sometimes, symptoms (like fever or swelling) linger not because the bacteria are thriving, but because your immune system is still in “fight mode.”
Example Scenarios
- A college student with strep throat, plenty of rest, and no other conditions: probably feels much better within 48 hours.
- Someone with diabetes dealing with a toenail infection: even with proper antibiotic use, improvement might take longer due to reduced circulation and slower healing.
And here’s something subtle — stress, sleep deprivation, even poor nutrition can shape how long does it take for amoxicillin to work. Your body’s defenses need support just as much as they need the antibiotic.
Pro Tip: Pairing antibiotics with healthy habits — hydration, sleep, balanced diet — sounds boring, but it’s surprisingly effective. It gives your immune system a fair chance to work with the medication instead of against it.
8. Form of Amoxicillin
Not all amoxicillin looks the same, and the form you take can influence how long does it take for amoxicillin to work.
Common Oral Formulations
- Amoxicillin capsule or tablet – The standard version most adults take. Reliable, steady absorption.
- Chewable tablets – Often prescribed for kids or anyone who struggles with swallowing pills.
- Liquid suspension – Measured by spoon or syringe, usually for children. Because it’s already dissolved, some people feel it kicks in a bit faster.
- Extended-release tablets – Designed for slow release, often for severe infections like bacterial pneumonia or sinus infection. These don’t work faster — they just keep steady levels over time.
- IV form (in hospitals) – Used for emergency medicine situations, like serious respiratory tract infections or septicemia. Relief can be more rapid since the drug bypasses digestion entirely.
Comparing Forms of Amoxicillin
| Form | Typical Use Case | Speed of Action | Notes |
| Capsule/Tablet | Adults, common infections | Standard (2–3 days for relief) | Most widely prescribed |
| Chewable tablets | Children, dental infections | Similar to tablets | Easy for kids |
| Liquid suspension | Kids, difficulty swallowing | May feel quicker | Needs refrigeration |
| Extended-release tablets | Severe respiratory/sinus infections | Slower but steady | Must take with food |
| IV (hospital use) | Life-threatening infections | Fastest onset | Monitored setting only |
Pro Tip: Don’t switch between formulations on your own. For example, replacing an extended-release tablet with standard capsules can totally change how the drug works in your system. Always stick with the prescribed course.
9. Compliance with Prescription
Honestly, this is where a lot of people slip up. Even if the infection is mild, how long does it take for amoxicillin to work often depends on whether you take it as prescribed.
Common Compliance Issues
- Stopping too early – You feel better after 2–3 days, so you stop. Problem is, the bacterial load isn’t fully cleared. Those surviving bacteria are often tougher — leading to antibiotic-resistant bacteria.
- Skipping doses – Life happens. But missing pills lowers the steady drug concentration in your system, which delays recovery.
- Doubling up after a missed dose – Doesn’t make the antibiotic work faster, just raises the risk of side effects like digestive complications or yeast infection.
- Not following food instructions – For instance, not taking extended-release tablets with food can reduce absorption.
Why Compliance Matters
Medication compliance isn’t just about you. The American Heart Association and Infectious Diseases experts warn that incomplete antibiotic use contributes to wider public health problems — more resistant bacterial strains, more complicated treatments, and higher healthcare costs.
Here’s a quick checklist to keep compliance simple:
- Take your amoxicillin at the same time every day.
- Finish the prescribed course, even if you feel better.
- Don’t share leftover pills (dosage regimens vary for a reason).
- Call your healthcare professional if side effects become intolerable — don’t just stop on your own.
Pro Tip: Set a phone alarm or use a medication tracking app. It sounds silly, but small reminders can make a huge difference in sticking with your treatment plan.
10. Underlying Medical Conditions
Not everyone’s body processes amoxicillin in the same way. If you’ve got certain medical conditions, the timeline of how long does it take for amoxicillin to work can slow down or become less predictable.
Conditions That May Affect Effectiveness
- Kidney disease – Amoxicillin is cleared through the kidneys. Reduced function can mean the drug lingers longer, which sometimes requires adjusted dosage regimens.
- Liver issues – While less common, severe liver problems can affect how the drug is metabolized.
- Diabetes – Slower healing and circulation issues may delay recovery from bacterial infections like gum disease or foot infections.
- Digestive disorders – Conditions like inflammatory bowel disease may increase side effects or reduce absorption of oral formulations.
- Immune-compromising illnesses – HIV, cancer, or autoimmune disorders can blunt the immune response, making the drug less effective on its own.
Conditions and Impact on Amoxicillin
| Medical Condition | Effect on Amoxicillin | Notes |
| Kidney disease | Slower clearance → higher drug levels | Dosage adjustments required |
| Liver disease | Altered metabolism | Monitor liver function |
| Diabetes | Slower healing | Risk of persistent infection |
| Digestive complications | Reduced absorption | May need an alternative form (IV) |
| Weak immune system | Delayed recovery | Immune support critical |
Pro Tip: If you have chronic health conditions, don’t just accept slower progress as “normal.” A healthcare professional may adjust your treatment plan or switch to another antibiotic class better suited for your situation.
When to Contact a Doctor?
Here’s where things get real. While many infections improve within that 2–3 day window, sometimes they don’t — and waiting too long can make matters worse. So, when do you actually pick up the phone (or use virtual urgent care)?
Red Flags to Watch For
- No improvement after 3–5 days – Could mean antibiotic-resistant bacteria or a misdiagnosis (like a viral infection instead).
- Worsening symptoms – Rising fever, spreading redness, new pain, or difficulty breathing.
- Allergic reactions – Rash, swelling, difficulty breathing (potential signs of penicillin allergy or, in rare cases, toxic epidermal necrolysis).
- Digestive complications – Severe diarrhea could point to Clostridium difficile (C. diff), which sometimes happens after antibiotic use.
- Recurrent infections – Infection clears but returns quickly, hinting at amoxicillin resistance or underlying immune system issues.
Situations That Require Urgent Care
- Signs of anaphylaxis (emergency medicine right away).
- Symptoms pointing toward C. diff infection (persistent, watery diarrhea).
- Chest pain, confusion, or extreme fatigue while on antibiotics.
Pro Tip: Don’t wait until the end of your prescribed course if something feels “off.” Doctors — whether at Cleveland Clinic, Mayo Clinic, or even your neighborhood urgent care — often say they’d rather hear from you early than deal with a serious complication later.
Conclusion
So, at the end of the day, the answer to how long does it take for amoxicillin to work isn’t just one number. For a lot of people, it’s somewhere between 48 and 72 hours before symptoms noticeably ease. But the whole story depends on so many moving parts — the type of infection, your dosage regimens, how strong your immune response is, even whether you remembered to take your extended-release tablets with food.
Most bacterial infections clear up when you finish the full prescribed course, but skipping pills, stopping early, or ignoring side effects can throw things off. And while amoxicillin is incredibly common — from strep throat to sinus infection to dental abscesses — it’s not a magic bullet. Viral infections, for example, won’t respond at all.
The safest takeaway? Be patient, finish your medication, and if something feels wrong — whether it’s no improvement after 3–5 days or a sudden allergic reaction — reach out to a healthcare professional. That could mean your family doctor, virtual urgent care, or even emergency medicine if it’s severe.
And maybe the bigger reminder is this: antibiotics are powerful, but they only work if we use them wisely. That means practicing antimicrobial stewardship — not pushing for antibiotics when we don’t need them, and respecting the prescribed course when we do.
People Also Ask
1. How do you know amoxicillin is working?
You’ll usually feel symptom relief within 2–3 days. Less pain, reduced fever, or easier breathing are good signs. If symptoms linger past day 3–4, check with your healthcare professional.
2. Can amoxicillin cause diarrhea?
Yes, mild diarrhea is one of the most common side effects. It happens because antibiotics disrupt normal gut bacteria. Staying hydrated and adding probiotics sometimes helps balance things.
3. How quickly does amoxicillin clear an infection?
Most infections improve within 48–72 hours, but full clearance depends on finishing the prescribed course. Stopping too early can let bacteria grow back stronger.
4. Is amoxicillin good for tooth abscess?
Yes, dentists often prescribe it for dental infections. But long-term relief may still require a root canal or extraction. Antibiotics alone can’t fix the root cause of an abscess.
5. What to avoid when taking amoxicillin?
Skip alcohol, acidic foods in excess, and don’t mix with certain drugs like blood thinners without medical advice. Always ask your doctor before combining it with other prescriptions.
6. What is the strongest antibiotic for bacterial infection?
It depends on the infection and bacterial strain. Broad-spectrum antibiotics like carbapenems or Augmentin are often stronger than plain amoxicillin. But “strongest” isn’t always the safest first choice.
7. What are three expected side effects of amoxicillin?
Nausea, diarrhea, and skin rash are the most common. Usually mild, but sometimes more serious allergic reactions can occur. Always watch for swelling or breathing problems as warning signs.
8. Can I take amoxicillin on an empty stomach?
Yes, standard amoxicillin can be taken without food. Extended-release tablets should always be taken with a meal. A light snack may also reduce the chance of nausea.
9. What happens if you accidentally take 2 amoxicillin 500mg?
One extra dose usually isn’t dangerous, but you might feel nausea or stomach upset. Contact your doctor if you’re unsure. Repeated overdosing, though, can stress your kidneys or gut.
10. How long does it take amoxicillin to clean your system?
It typically leaves the body within 24 hours after your last dose. But in people with kidney issues, it may take longer. That’s why dosing schedules differ for certain conditions.



