It’s strange how often people use the words cellulite and lipedema as if they mean the same thing. You might’ve done it too — looked in the mirror, noticed the uneven skin texture on your thighs, and wondered, “Is this just cellulite… or something else?” That’s exactly where the confusion begins.
The difference between cellulite and lipedema isn’t just about how your skin looks; it’s about what’s happening deep under it — in the connective tissue, fat cells, and lymphatic system that quietly shape your body’s landscape.
Most people think cellulite is purely a cosmetic concern — those dimples that resemble an orange peel texture. But lipedema? It’s far more complex. It’s a chronic, often painful disorder of fat distribution, usually affecting the legs, hips, and sometimes arms, but sparing the hands and feet.
While cellulite sits on the surface, lipedema builds deep — creating symmetrical fat buildup that doesn’t respond to diet or exercise. And yet, both conditions share the same emotional terrain: frustration, confusion, and that uneasy feeling of being misunderstood — even by doctors.
Early awareness of lipedema is crucial because catching it before it progresses can make all the difference. With the right lipedema treatment — from compression therapy to manual lymphatic drainage — people can manage symptoms, reduce swelling, and reclaim comfort in their own bodies.
What Is Cellulite? (The Common Skin Dimpling Explained)

Let’s start with what cellulite actually is — because despite being so common, it’s still wildly misunderstood. At its simplest, cellulite is a harmless condition where fat cells push through the fibrous connective tissue beneath the skin.
This creates that familiar dimpled appearance, often called orange peel or cottage cheese texture. While the word might sound clinical, the experience is anything but — especially when society treats it as a flaw rather than just a normal part of skin structure.
The Science Behind Cellulite Formation
Underneath your skin lies a network of collagen fibers that connect the skin to deeper fat tissue. When these fibers tighten or weaken unevenly, pockets of adipose tissue (fat) bulge through — creating a textured surface.
Hormonal changes, particularly shifts in estrogen, influence circulation and collagen integrity, making cellulite more visible in women than men. Genetics also play a quiet but powerful role; if your mother or grandmother had it, chances are, you will too.
Why women are more prone:
- Their connective tissue structure runs vertically, making it easier for fat deposits to push through.
- Men’s tissue, by contrast, forms a crisscross pattern — offering more resistance.
- Fluctuations during puberty, pregnancy, and menopause can trigger visible changes in skin elasticity.
Common Areas and Stages of Cellulite
Cellulite tends to appear where fat distribution is naturally higher — thighs, buttocks, hips, and sometimes arms. It develops in stages:
| Grade | Visible Appearance | Details |
| Stage 1 | Smooth skin while standing; dimples visible when pinched. | Early stage; minor connective tissue tension. |
| Stage 2 | Dimples visible while standing. | Fat pockets push against weakened collagen. |
| Stage 3 | Deep depressions, visible even when lying down. | Reduced circulation and loss of skin elasticity. |
And here’s the thing — it’s not necessarily tied to your weight. Even lean, athletic women can have cellulite because it’s about skin structure, not body fat percentage.
Many turn to cellulite treatment options like massage techniques, acoustic wave therapy, or laser procedures to smooth the texture, while others focus on anti-inflammatory diets and exercise regimens to boost circulation.
The right choice depends on your body’s response — and your patience, because real results take time.
Pro Tip: Think less about “erasing” cellulite and more about supporting your connective tissue. Staying hydrated, eating foods rich in antioxidants, and doing lymphatic drainage massage can improve elasticity naturally.
What Is Lipedema? (The Often-Misdiagnosed Fat Disorder)
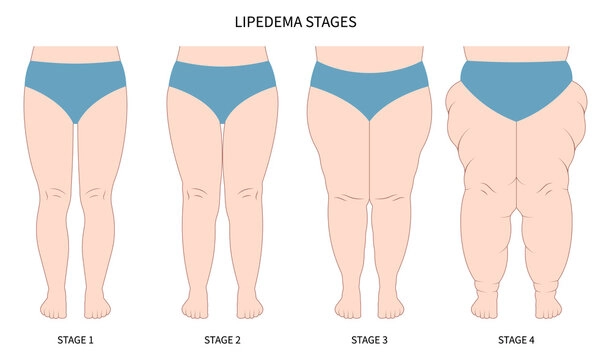
Now, lipedema — this one’s tricky. Because for years, people (and even some doctors) brushed it off as just “stubborn fat.” But lipedema isn’t about laziness or lifestyle choices. It’s a chronic fat disorder — an inflammatory condition that mainly affects women, usually in the legs, thighs, hips, and sometimes the arms.
You’ll hear terms like lipedema legs or lipedema disease tossed around, but underneath, it’s a medical reality tied to hormonal changes, connective tissue fragility, and a dysfunctional lymphatic system.
When you compare it to cellulite, the difference between cellulite and lipedema becomes more obvious — cellulite affects the skin’s surface, while lipedema affects fat cells deep within adipose tissue, leading to symmetrical fat buildup that resists diet and exercise. It often starts after hormonal milestones — puberty, pregnancy, or menopause — and worsens slowly over time.
Understanding Lipedema’s Root Cause
Doctors still don’t know everything about lipedema, but research in places like Deutsches Ärzteblatt International and the American Society for Plastic Surgery suggests strong hormonal and genetic links.
Estrogen seems to play a central role in how fat tissue is distributed and retained. Some experts believe connective tissues in women with lipedema hold excess tissue sodium content, leading to water retention and swelling.
Key Triggers of Lipedema:
- Hormonal fluctuations (puberty, pregnancy, menopause)
- Genetic predisposition — if your mother or sister has it, you’re more likely to develop it
- Lymphatic system dysfunction, slowing drainage and causing inflammation
- Reduced mobility and chronic pain as the disease progresses
Lipedema typically causes symmetrical swollen legs (sometimes called “trunk-like legs”) that feel tender or painful to the touch. What’s heartbreaking is how often people are misdiagnosed with obesity, told to “just lose weight,” when lipedema doesn’t respond to calorie restriction or even bariatric surgery.
Pro Tip: If you notice disproportionate fat accumulation below the waist — especially with pain, bruising, or heaviness — ask about a lipedema diagnosis. A board-certified plastic surgeon or vascular specialist familiar with S1 guidelines can help confirm it using CT scans, DEXA scans, or nuclear medicine imaging to rule out orthopedic causes.
10 Key Differences Between Cellulite and Lipedema
Here’s where we break it down clearly — side by side. Because while both involve fat, the difference between cellulite and lipedema runs far deeper than appearance. Cellulite is about skin structure and collagen fibers, while lipedema is about fat distribution and lymphatic dysfunction.
Below is a simple comparison chart — it’s not meant to medicalize you, just to make things click a little easier:
| Feature | Cellulite | Lipedema |
| Cause | Fibrous connective tissue pulling down on skin, creating dimples | Chronic, inflammatory fat disorder affecting adipose tissue |
| Appearance | Dimpled or “orange peel” texture | Column-like swelling; symmetrical fat buildup on legs and arms |
| Pain | Usually painless | Painful to touch; may cause chronic pain and tenderness |
| Location | Buttocks, thighs, hips | Legs, thighs, arms — but spares hands and feet |
| Gender | 85–90% women | Almost exclusively women |
| Progression | Cosmetic; doesn’t worsen with time | Progressive and can cause mobility issues |
| Treatment | Lifestyle changes, massage techniques, laser treatment, topical treatments | Compression therapy, manual lymphatic drainage, lipedema surgery, or Complete Decongestive Therapy (CDT) |
| Hormonal Role | Moderate influence (estrogen) | Strong hormonal and genetic connection |
| Genetic Link | Moderate | Strong hereditary component |
| Mobility Impact | None | May restrict movement due to fibrous fat and swelling |
While cellulite might respond to cellulite treatment options like acoustic wave therapy, vacuum-assisted tissue release, or radiofrequency treatment, lipedema often requires medical management with compression garments, pneumatic compression devices like the Flexitouch Plus system, and sometimes surgical intervention such as liposuction or surgical debulking.
And here’s a truth few mention — the emotional impact. Many women with lipedema develop body image struggles or feel judged because people assume it’s just weight gain. But once you recognize it for what it really is, that knowledge can be freeing — even empowering.
Pro Tip: If your legs feel heavy or tender at the end of the day — or your fat deposits are symmetrical and stop abruptly at the ankles (creating a “cuff effect”) — it’s worth consulting a lipedema team. Early intervention with compression therapy guidance or manual lymphatic drainage can slow progression dramatically.
Causes of Cellulite vs Lipedema — What Science Says

If you’ve ever wondered why one person develops deep skin dimpling while another ends up with swollen, weak or heavy painful legs, the answer lies in how hormones, connective tissue, and the lymphatic system work together—or sometimes, fail to.
The difference between cellulite and lipedema really starts with what’s happening under the surface, where fat cells, collagen fibers, and circulation quietly shape what you see in the mirror.
Both conditions share some triggers—like hormonal changes, genetic factors, and poor lymphatic drainage—but the mechanisms differ. Cellulite is mainly structural, while lipedema is inflammatory and progressive. Let’s break it down.
Hormonal & Genetic Factors
Hormones—especially estrogen—play a starring role in both cellulite and lipedema. Estrogen affects fat distribution, collagen production, and vascular health, explaining why these conditions are so much more common in women.
When estrogen levels fluctuate (during puberty, pregnancy, or menopause), it can lead to weakened connective tissue and water retention. This allows adipose tissue to expand and form either surface dimples (cellulite) or deep, fibrous fat deposits (lipedema).
Genetic predisposition is another quiet but powerful driver. If your family has a history of symmetrical fat buildup, hormonal imbalance, or circulatory issues, you’re more likely to experience one—or both—conditions. Research shows that women with lipedema often share markers in genes linked to inflammation and tissue sodium content.
Here’s a quick overview:
| Factor | Cellulite | Lipedema |
| Primary Mechanism | Structural (skin + connective tissue) | Inflammatory (fat tissue + lymphatic system) |
| Hormonal Influence | Estrogen impacts collagen and fat storage | Estrogen triggers abnormal fat accumulation |
| Genetic Link | Moderate; linked to collagen genes | Strong; family clusters are common |
| Tissue Affected | Superficial fat layer | Deep subcutaneous fat and lymphatic vessels |
| Inflammation Level | Mild, localized | Chronic and systemic |
Pro Tip: Chronic inflammation fuels both cellulite and lipedema. Try incorporating an anti-inflammatory diet—think omega-3s, leafy greens, berries, and turmeric. It won’t “cure” either condition, but it helps reduce swelling, improve lymph flow, and support collagen health.
Lifestyle & Environmental Influences
Lifestyle doesn’t cause lipedema, but it can influence its progression. Sedentary habits, tight clothing that restricts lymph drainage, and high-sodium diets can all worsen swelling. For cellulite, factors like poor circulation, smoking, stress, and lack of muscle tone tend to make the skin’s surface texture more visible.
Other contributors include:
- Environmental toxins that interfere with hormonal balance
- Dehydration, which reduces skin elasticity
- Rapid weight fluctuations, straining connective tissues
- Inflammatory foods (sugar, processed carbs, alcohol)
- Stress hormones (cortisol) that affect fat storage
How Cellulite and Lipedema Are Diagnosed
Here’s where things often go wrong. Most women with lipedema spend years being told they just need to lose weight. Others are dismissed because their condition “looks like normal cellulite.”
The difference between cellulite and lipedema becomes critical at this stage—because while cellulite is a cosmetic issue, lipedema is a medical condition that needs professional management.
Recognizing When It’s Not Just Cellulite
If you’ve been trying cellulite treatments—like dry brushing, radiofrequency treatment, or skin-tightening creams—and nothing changes (or the swelling worsens), that’s a red flag.
Unlike cellulite, lipedema causes symmetrical swelling that doesn’t affect the feet, feels painful or tender, and may bruise easily. The fat tissue in lipedema also has a denser, “rubbery” feel compared to the soft texture of cellulite.
Signs you might be dealing with lipedema instead of cellulite:
- Persistent heaviness or tightness in the legs or arms
- Easy bruising and tenderness when pressure is applied
- Swelling that worsens with standing or heat
- Fat deposits that stop abruptly at the ankles (the “cuff effect”)
- No improvement from weight loss or exercise
If any of these sound familiar, it’s worth getting a lipedema diagnosis from a trained professional—ideally one experienced in vascular medicine or lymphatic disorders.
Pro Tip: Keep a symptom journal. Track swelling, tenderness, and daily activity. This can help your doctor differentiate between cellulite, lipedema, and other lymphatic or orthopedic causes.
Tests and Medical Evaluation
Diagnosing cellulite is mostly visual, based on skin texture and grading (Stage 1–3). Lipedema, however, requires a clinical examination and sometimes imaging to confirm. A board-certified plastic surgeon or vascular specialist may order:
- Ultrasound or MRI – to assess fat distribution and tissue density
- CT scans or DEXA scans – to measure adipose tissue thickness
- Lymphoscintigraphy or nuclear medicine imaging – to evaluate lymphatic flow
- Family history review – to identify genetic components
Some advanced centers, like North Shore University Hospital or Long Island Jewish Medical Center, even use nuclear imaging to detect lymphatic blockages before symptoms worsen.
| Diagnostic Tool | Used For | Primary Goal |
| Visual Exam | Cellulite | Assess texture and severity |
| Ultrasound / MRI | Lipedema | Identify deep fat buildup and inflammation |
| DEXA / CT Scan | Both | Analyze fat distribution |
| Lymphoscintigraphy | Lipedema | Evaluate lymphatic system function |
Treatment Options for Cellulite
Cellulite might be harmless, but that doesn’t make it easy to live with. The difference between cellulite and lipedema becomes especially visible in treatment — cellulite responds to cosmetic and lifestyle therapies, while lipedema requires medical management.
If you’ve ever stared at the mirror after trying countless anti-cellulite treatments, you’re not alone. Millions of women chase smoother skin through creams, massages, and dietary tweaks — and while some methods help, others are little more than marketing.
Still, real science does exist behind what works. Let’s start simple.
Topical & Non-Invasive Treatments
Cellulite forms when fat cells push against weakened collagen fibers, creating that “orange peel” or cottage cheese texture. So, the most effective treatments target the skin structure, collagen repair, and circulation.
Common Cellulite Treatments That Show Results:
- Retinol-based creams: Improve collagen production and skin elasticity.
- Caffeine scrubs or gels: Stimulate circulation and help drain excess fluid from connective tissues.
- Laser treatments & radiofrequency treatment: Heat the deeper layers of fat tissue, tightening skin and boosting collagen.
- Acoustic wave therapy: Uses vibrations to break down fibrous fat bands, reducing dimpling.
- Vacuum-assisted precise tissue release: Mechanically loosens tight collagen fibers, improving the skin’s smoothness.
Pro Tip: Combine your topical treatments with lymphatic drainage massage or Myofascial Release techniques to enhance circulation. A good compression garment can help maintain the results longer by reducing fluid buildup.
Exercise, Diet, and Circulation Boosters
You’ve probably heard the phrase “you can’t out-train cellulite.” And it’s partly true — but movement still helps. Regular exercise regimens improve blood flow, lymphatic drainage, and muscle tone, all of which make dimples less visible.
Best Exercises for Reducing Cellulite Appearance:
- Strength training: Builds muscle to support the overlying fat and skin.
- High-Intensity Interval Training (HIIT): Burns stored fat and improves circulation.
- Walking or swimming: Gentle ways to boost lymph drainage and oxygen flow.
Diet matters too — especially when it comes to inflammation. A low-sodium, anti-inflammatory diet rich in omega-3s, antioxidants, and hydration can reduce fluid retention and strengthen skin structure.
Sample Anti-Inflammatory Foods Table:
| Eat More Of | Avoid / Limit |
| Leafy greens, berries, citrus fruits | Processed meats, fried foods |
| Fatty fish (salmon, sardines) | Refined sugar and carbs |
| Green tea, turmeric, ginger | Alcohol, caffeine excess |
| Nuts and seeds | High-sodium snacks |
Treatment Options for Lipedema
Now, here’s where the path diverges sharply. Unlike cellulite, lipedema treatment is medical — not cosmetic. You can’t “massage” it away or sweat it off. It’s a chronic condition that requires a mix of compression therapy, manual lymphatic drainage, and in some cases, lipedema surgery or surgical debulking. The focus isn’t on looks — it’s on reducing pain, inflammation, and fat buildup, and improving mobility.
Medical Interventions
Lipedema often needs a multidisciplinary approach — think of it as teamwork between vascular specialists, physical therapists, and plastic surgeons. According to the American College of Cardiology and American Heart Association, early medical management can drastically slow its progression.
Common Medical Treatments for Lipedema:
- Tumescent liposuction: A precise, fluid-based technique that removes abnormal adipose tissue while preserving lymphatic vessels.
- Water-jet assisted liposuction: Gentler, ideal for stages 1 and 2 lipedema with minimal fibrosis.
- Compression garments & compression stockings: Help manage swelling and improve lymphatic flow.
- Pneumatic compression devices (e.g., Flexitouch Plus system): Provide automated massage to promote lymph drainage.
- Complete Decongestive Therapy (CDT): Combines manual lymphatic drainage, skin moisturizers, and bandaging to control swelling and tenderness.
Pro Tip: Always consult a board-certified plastic surgeon or a lipedema team before opting for surgery. It’s not cosmetic liposuction — it’s specialized treatment requiring lymphatic preservation techniques.
Supportive Lifestyle & Self-Care
Medical care helps manage the physical side — but day-to-day habits shape your long-term comfort. Simple, sustainable choices often make the biggest difference:
Lifestyle Habits to Support Lipedema Management:
- Gentle movement: Low-impact exercises like swimming, yoga, or cycling reduce stiffness without stressing joints.
- Anti-inflammatory diet: Focus on whole foods — leafy greens, lean protein, berries, olive oil.
- Compression therapy guidance: Use fitted garments (with help from occupational therapy or Advanced Rehabilitation Services) to reduce discomfort.
- Emotional support: Online lipedema groups can help with body image acceptance and pain management strategies.
- Massage & lymph drainage: Regular manual lymphatic drainage sessions can ease swelling and tenderness.
Lifestyle Tip: Some patients find that Customized Exercise Plans—guided by physiotherapists—help improve circulation without overexerting swollen limbs.
Managing Emotional Health and Body Confidence
The difference between cellulite and lipedema isn’t just physical — it’s deeply emotional. Many women share how years of frustration, pain, and body-image struggles often hurt more than the conditions themselves.
Whether you’re dealing with cellulite dimples or lipedema swelling, that mirror moment can stir up shame, confusion, or even hopelessness. But let’s talk about something often overlooked — your emotional health deserves as much care as your skin or lymphatic system.
Living with visible texture changes or disproportionate fat distribution can chip away at self-esteem. People often misinterpret lipedema as obesity or assume cellulite is just a sign of poor fitness — and that misunderstanding leads to stigma.
But here’s the truth: neither has anything to do with laziness or neglect. These are biological and hormonal conditions tied to connective tissue health, genetics, and sometimes lymphatic dysfunction.
Ways to Strengthen Body Confidence and Emotional Health:
- Acknowledge the facts: Cellulite affects 80–90% of women; lipedema impacts nearly 11%. You’re not alone.
- Avoid comparison traps: Your body tells a different story — one of resilience, not failure.
- Find supportive communities: Online lipedema groups or body-positivity forums help normalize shared experiences.
- Try gentle self-care rituals: Dry brushing, warm baths, or light stretching help reconnect you to your body compassionately.
- Professional help: A therapist familiar with chronic pain or body dysmorphia can help reframe internal dialogue.
Pro Tip: Focus less on “fixing” your appearance and more on managing symptoms and building comfort. Healing your relationship with your body is as essential as any physical treatment.
If you’ve ever hidden your legs in summer or avoided certain clothes, you’re not being vain — you’re reacting to years of societal pressure. But here’s a small shift: when you treat your condition with awareness, not shame, healing starts to feel lighter.
Prevention & Early Awareness Tips
Early understanding can change everything. Recognizing the difference between cellulite and lipedema early helps you act faster — and with the right strategy.
While cellulite is more of a skin-texture concern, lipedema progresses if left untreated, leading to painful fat buildup, mobility issues, and chronic swelling. Awareness isn’t just prevention — it’s empowerment.
Let’s break it down a bit.
Early Warning Signs to Watch For:
| Cellulite | Lipedema |
| Mild dimpling, especially around thighs and buttocks | Bilateral swelling in legs or arms, even with diet/exercise |
| Texture changes — like orange peel or cottage cheese | Pain, tenderness, or bruising without clear cause |
| Usually soft and painless | Heavy, cold, or tight sensation in limbs |
| Often linked to hormones, inactivity, or poor circulation | Often triggered by hormonal shifts (puberty, pregnancy, menopause) |
If you spot symmetrical swelling, pain when pressing fat tissue, or skin tenderness, don’t wait — get evaluated by a vascular or lymphatic specialist. Lipedema caught early responds far better to compression therapy, manual drainage, and dietary adjustments.
Simple Prevention & Management Habits
- Stay active: Gentle daily movement promotes lymphatic flow.
- Maintain hydration: Water supports your connective tissue integrity.
- Follow anti-inflammatory eating habits: Focus on omega-3s, greens, and citrus-rich antioxidants.
- Wear compression garments if needed: Especially during travel or prolonged standing.
- Get regular checkups: Annual body composition assessments can detect early fluid retention.
Pro Tip: Don’t confuse stubborn cellulite with lipedema swelling. If your “fat” feels painful, cold, or bruises easily — it’s worth a professional opinion.
Ultimately, understanding the signs allows you to take control before symptoms escalate. Awareness doesn’t just protect your health — it protects your peace of mind.
Key Takeaways: What Really Sets Them Apart
After diving deep into symptoms, causes, and treatments, let’s simplify the difference between cellulite and lipedema once and for all. They may look similar on the surface — uneven fat distribution, skin dimpling, swelling — but biologically, they’re worlds apart.
Cellulite is mostly cosmetic, caused by fat pushing through weakened connective tissue, leading to that uneven skin texture. It’s influenced by hormones, genetics, and lifestyle factors like inactivity or circulation issues.
Lipedema, however, is a chronic fat disorder involving symmetrical fat buildup, usually in the legs or arms, that doesn’t respond to diet or exercise. It’s painful, progressive, and tied to hormonal and lymphatic dysfunction.
Here’s a quick comparison for clarity:
| Aspect | Cellulite | Lipedema |
| Nature | Cosmetic skin condition | Chronic fat distribution disorder |
| Affected Area | Thighs, hips, buttocks | Legs, hips, arms (bilaterally) |
| Pain or Tenderness | Usually painless | Painful and tender to touch |
| Response to Exercise/Diet | Can improve with diet & fitness | No improvement with exercise or calorie restriction |
| Cause | Weak connective tissue & trapped fat cells | Hormonal, genetic, and lymphatic dysfunction |
| Treatment Focus | Collagen repair, skin tightening, fat reduction | Compression therapy, lymphatic drainage, lipedema surgery |
| Emotional Impact | Body image concern | Chronic pain, mobility issues, emotional distress |
Pro Tip: If your “cellulite” feels sore, heavy, or bruises easily — it may not be cellulite at all. Seek a vascular or lymphatic specialist for a proper diagnosis. Early detection of lipedema symptoms can prevent long-term complications.
Ultimately, the most important takeaway is this: cellulite may affect your confidence, but lipedema affects your quality of life. Understanding this distinction helps you choose better care — not just the right cream or workout, but the right medical guidance.
Conclusion
The difference between cellulite and lipedema goes far deeper than what shows up on your skin — it’s about learning to understand, care for, and reconnect with your body. Both remind us that health isn’t just surface-level; it’s emotional, hormonal, and deeply personal.
When you start listening to what your body’s been trying to tell you — whether it’s through uneven skin texture, tenderness, or swelling — you move toward healing that’s more compassionate than cosmetic.
If you’ve spent years chasing smooth skin or fighting stubborn fat, maybe it’s time to shift focus. The difference between cellulite and lipedema lies not only in their causes but also in how we respond.
From laser and acoustic wave therapy to compression treatment and lymphatic drainage, the real progress begins with awareness. When you treat both conditions with empathy and informed care, you’re not just improving your skin — you’re honoring your body’s story, one mindful step at a time.
Frequently Asked Questions
1. What is the main difference between cellulite and lipedema?
Cellulite is a cosmetic skin dimpling issue, while lipedema is a painful fat disorder caused by lymphatic and hormonal imbalance. Understanding the difference between cellulite and lipedema helps guide proper diagnosis and effective treatment choices.
2. Can exercise get rid of lipedema?
No, lipedema fat doesn’t respond to diet or exercise. However, gentle movement helps improve circulation and reduce pain. Low-impact exercises like swimming or walking can also boost lymphatic drainage and support overall mobility.
3. Does cellulite mean you’re overweight?
Not at all. Even lean individuals can have cellulite — it’s tied to connective tissue structure, not body fat percentage. Maintaining hydration and a balanced diet rich in antioxidants can help reduce visible fat deposits over time.
4. What are early signs of lipedema?
Tender, symmetrical swelling in the legs or arms that feels cold, bruises easily, and doesn’t reduce with weight loss. These symptoms often appear around hormonal changes such as puberty, pregnancy, or menopause.
5. How can I tell if my cellulite is actually lipedema?
If it’s painful, symmetrical, and accompanied by swelling, seek an evaluation from a vascular or lymphatic specialist. A proper lipedema diagnosis often involves physical exams, imaging scans, and reviewing your family history.
6. Can lipedema be cured permanently?
There’s no complete cure yet, but liposuction, compression therapy, and lifestyle support can manage symptoms effectively. Following an anti-inflammatory diet and wearing compression garments can help prevent symptom progression.
7. Are cellulite treatments safe for lipedema patients?
Not always — treatments like radiofrequency or laser therapy can worsen inflammation. Always consult your doctor first. Your healthcare provider may recommend manual lymphatic drainage or vacuum-assisted tissue release instead.
8. What foods help reduce cellulite naturally?
Antioxidant-rich foods — like berries, leafy greens, citrus fruits, and green tea — support collagen and circulation. Adding omega-3 fats and vitamin C–rich meals may also strengthen connective tissues and enhance skin elasticity.
9. Why is lipedema often misdiagnosed as obesity?
Because both involve fat accumulation, but lipedema fat is resistant to calorie restriction and linked to lymphatic dysfunction. That’s why knowing the difference between cellulite and lipedema is vital for getting proper medical attention early.
10. Can men have cellulite or lipedema?
Cellulite occasionally, yes — but lipedema is almost exclusively found in women due to hormonal differences. Men may still experience connective tissue weakening or skin texture changes linked to lifestyle and genetics.



