If you’ve ever felt that sharp, uncomfortable burning tip of urethra no std kind of pain, you probably know how instantly worrying it feels. Your brain might immediately jump to the worst possibilities — sexually transmitted diseases, hidden infections, something serious.
But here’s the thing: not every burning sensation down there has anything to do with STDs. In fact, there are dozens of other explanations, ranging from very simple lifestyle selfcare tips (like not drinking enough water) to more medical conditions that sound scarier than they usually are.
And that’s what we’re digging into here — the less obvious but very real reasons why your urethra might burn even when tests for sexually transmitted infections come back clear. Some of them are temporary annoyances, others need proper treatment. Either way, understanding the possibilities helps you stop panicking and start asking better medical questions if the burning doesn’t go away.
(Quick pause — I should probably say: none of this replaces advice from a health professional. It’s more of a “here’s what could be going on” guide, so you have a framework before you end up deep in late-night internet rabbit holes.)
1. Urinary Tract Infection (UTI) Without STD
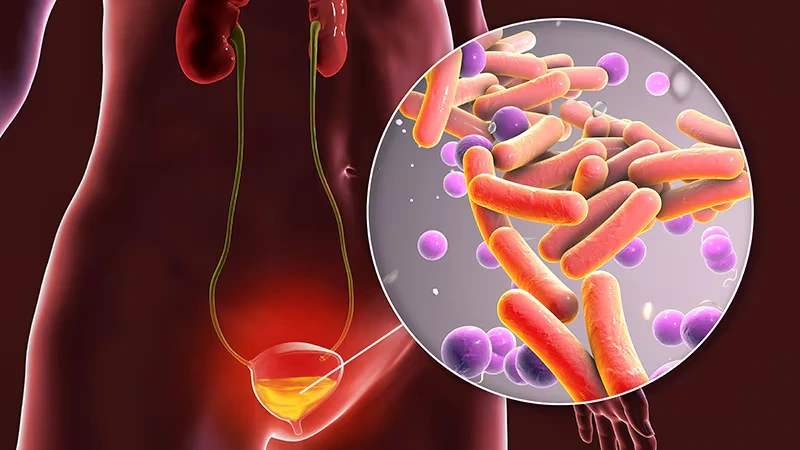
You’ve likely heard of UTIs — they’re incredibly common, especially among women but also in men. And yes, a UTI can absolutely cause painful urination, that annoying urgency to pee every few minutes, and sometimes even cloudy or strange-smelling urine… all without being tied to an STD.
What’s happening is pretty straightforward: bacteria sneak their way into the urinary tract, usually through the urethra, and set up shop. The bladder and urethra get irritated, inflamed, and in turn, you feel that uncomfortable burning sensation.
Common symptoms of a UTI include:
- A burning feeling when you urinate
- The need to pee constantly, even if only drops come out
- Cloudy or reddish urine (blood sometimes shows up)
- Pressure or pain in the lower belly
👉 Pro tip: If you’ve ever wondered, “Can I have a UTI without an STD?” the answer is a firm yes. They’re completely separate things. A urine test (or urine culture if it’s persistent) is usually what confirms it.
Small table for quick comparison:
| UTI (Non-STD) | STD-related infection |
| Bacteria are usually from the gut (E. coli) | Bacteria/viruses spread sexually |
| Burning + urgency, sometimes blood | Burning + discharge or sores possible |
| Treated with antibiotics | Needs specific STI treatment |
So, if the pain feels familiar, frequent, and it’s paired with that bathroom urgency, don’t panic about STDs. A simple bladder infection kill you or be the culprit.
2. Urethritis from Non-STD Causes
Now, here’s where it gets a little trickier. Urethritis is just a fancy word for inflammation of the urethra. And while many people assume it’s only tied to infections like chlamydia or gonorrhea, there’s a whole category called nonspecific urethritis.
This can happen from:
- Bacterial irritation that isn’t a classic STD
- Fungal infections
- Even something chemical, like swimming in heavily chlorinated pools or using a new soap that your body doesn’t like
Ever hopped out of a pool and noticed a weird stinging feeling when you pee? That’s urethral irritation, and it can mimic the burning you’d expect from an infection.
Some cases fall under urethral syndrome — where lab tests don’t show a clear bacterial cause, but the symptoms (burning, painful urination, maybe pelvic pain) are still very real. Doctors sometimes use tests like nucleic acid amplification testing or urine dipsticks to rule things out, but not everything shows up clearly.
(Honestly, it can be frustrating. One time after a long beach trip, I felt this stinging for days and convinced myself it was an infection. It wasn’t — just too much time in salty water and sunscreen-soaked swimsuits. Annoying but not dangerous.)
So yes, urethritis no std is a thing, and it’s worth considering if the discomfort pops up after certain activities rather than out of the blue.
3. Kidney Stones and Urinary Crystals
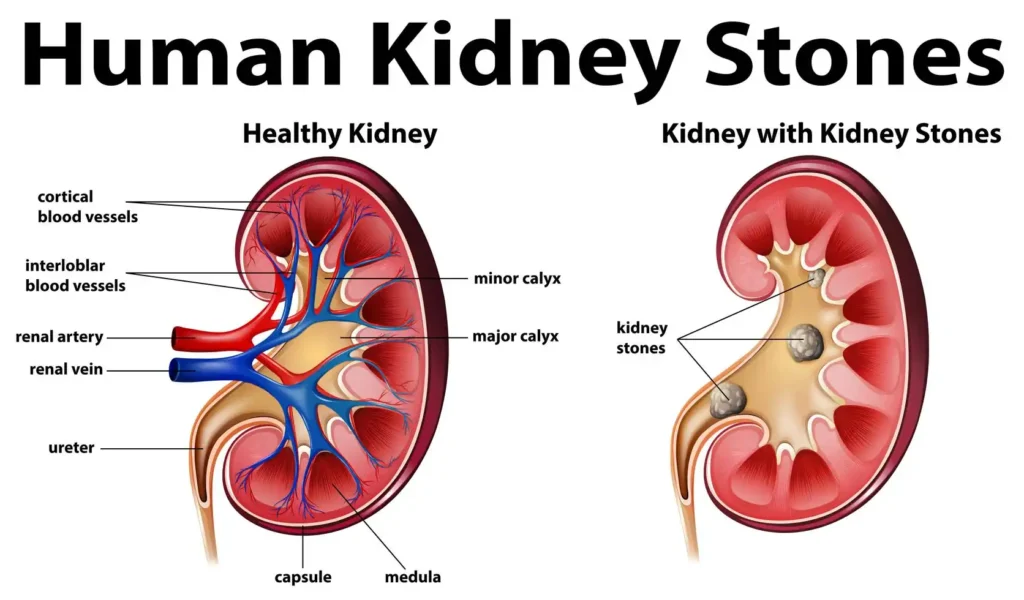
Kidney stones are one of those things you hope you’ll never experience… until you do. And honestly, they can make the burning tip of urethra no std issue feel ten times worse because the pain isn’t just at the end — it’s often radiating through your whole urinary tract.
Here’s what happens: tiny crystals (usually made of calcium or uric acid) form in your kidneys. Sometimes they stay small and pass unnoticed, but other times they grow into sharp stones that scrape the inside of your urinary tract. That scraping? Yeah, that’s why it feels like fire when you pee.
Other signs that kidney stones may be the cause:
- Sharp pain in the side or back (often called flank pain)
- Blood in the urine (it may look pink or reddish)
- Nausea or vomiting when the pain is intense
- Frequent trips to the bathroom with only small amounts of urine
Doctors often confirm stones with imaging, like a CT scan, pelvic ultrasound, or sometimes a retrograde pyelogram if they want a closer look at the ureters. Treatment can be as simple as pain management and hydration, or as high-tech as extracorporeal shock wave lithotripsy (ESWL), where they literally use sound waves to break the stone into passable pieces.
Quick comparison:
| Small Crystals | Larger Stones |
| May pass unnoticed | Cause severe flank pain |
| Burning when peeing | Blockage, possible infection |
| Managed with fluids | May need ESWL or surgery |
👉 Pro tip: If you ever feel both burning and see blood in your urine, don’t just brush it off as dehydration. Stones or even bladder inflammation could be behind it, and those need proper medical evaluation.
4. Dehydration and Concentrated Urine
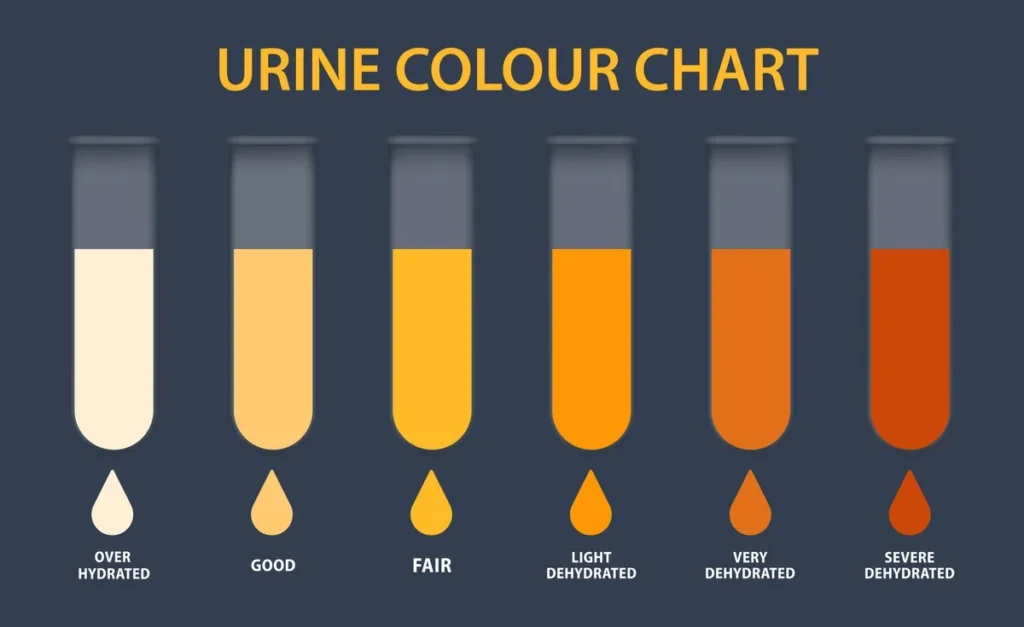
This one’s surprisingly common and (thankfully) easier to fix. When you don’t drink enough water, your urine becomes darker, more acidic, and, well… harsher on the lining of your urethra. That alone can lead to a burning sensation even though there’s no infection, no STD, nothing more sinister. Just too little fluid.
Think about it: athletes after a long workout, travelers on hot days, even office workers who can drink coffee instead of water — they’re all prone to this. You might pee and immediately think something’s wrong because of the sting, when it’s really just your body saying, “Hey, can I get a glass of water here?”
Typical signs dehydration is to blame:
- Dark yellow or amber-colored urine
- Dry mouth or headache along with urinary symptoms
- Strong-smelling urine
- Symptoms improve after a few hours of hydration
Hydration also matters for kidney health, bladder inflammation, and even preventing urinary tract infections. Doctors often emphasize lifestyle changes like drinking more fluids, cutting back on caffeine, and balancing electrolytes (sometimes with calcium glycerophosphate supplements) to make urine less irritating.
Quick list of drinks that help:
- Plain water (still the best)
- Diluted fruit juices (without added sugar)
- Herbal teas like chamomile or ginger
Drinks that hurt (more acidic, irritating):
- Coffee (too much can dehydrate)
- Alcohol (diuretic effect)
- Soda or energy drinks (acidic, full of sugar)
So if your urethra burns only after long periods of not drinking water or after heavy coffee days, dehydration might be the surprisingly simple explanation.
5. Prostatitis (Men-Specific)
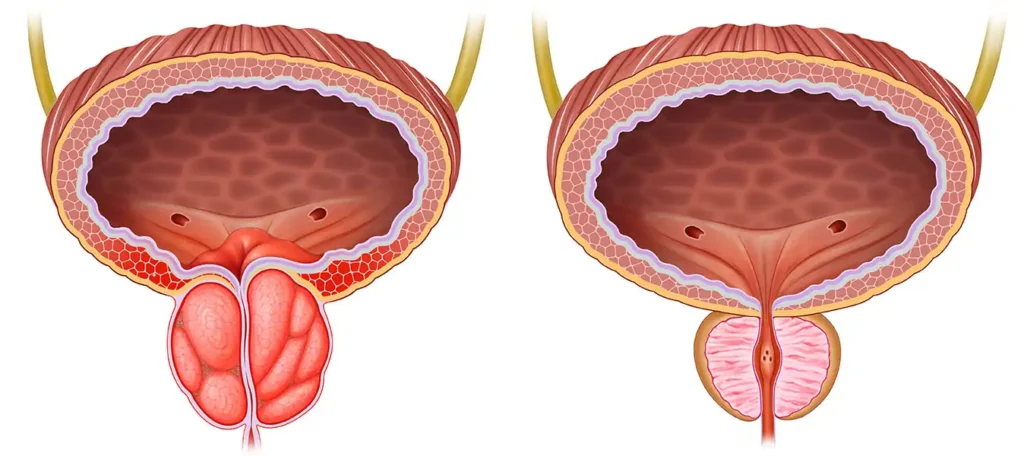
For men, one of the less talked about reasons for a burning tip of urethra no std is prostatitis — inflammation of the prostate gland. And honestly, it can be tricky because it comes in different forms: acute (sudden, severe) and chronic (lingering, sometimes subtle).
The prostate sits just below the bladder, wrapped around the urethra like a collar. So when it swells, the urethra gets squeezed. That pressure alone can cause painful urination, pelvic pain, or the feeling that you never fully emptied your bladder.
Symptoms often linked with prostatitis:
- Burning when urinating
- Dull ache between the scrotum and rectum
- Frequent trips to the bathroom at night
- Sometimes, fever or flu-like symptoms, if it’s an acute case
Doctors may check with urine culture, lab tests of discharge, or even imaging like an MRI of the pelvis if the pain won’t go away. Chronic prostatitis can sometimes overlap with benign prostatic hyperplasia (BPH) — another condition where the prostate enlarges with age and adds urinary symptoms into the mix.
Small comparison table:
| Acute Prostatitis | Chronic Prostatitis |
| Sudden onset, fever, chills | Long-term, low-grade discomfort |
| Requires prescription antibiotics | Managed with meds + lifestyle changes |
| Painful urination + pelvic pain | Urinary frequency, urethral pain |
👉 Pro tip: Some men ignore prostate issues because they don’t want awkward doctor visits, but catching them early can prevent bigger complications — including links to bladder cancer or, rarely, prostate cancer.
6. Vaginal or Vulvar Irritation (Women-Specific)
Women aren’t off the hook here either. Burning at the tip of the urethra (no STD in sight) can come from irritation around the vaginal and vulvar tissues. These tissues sit right next to the urethra, so when something is inflamed — yeast infections, bacterial vaginosis, or even dryness from hormonal changes — the urethra often feels the sting too.
Some women notice burning after sex, especially if there’s friction, low lubrication, or even a reaction to condoms or lubricants. Others get it during shifts in hormones, like menopause, when vaginal changes make the tissues thinner and more sensitive.
Possible culprits include:
- Yeast infections (itching + white discharge)
- Bacterial vaginosis (fishy odor + thin discharge)
- Hormonal shifts (post-menopause, pregnancy, birth control pills)
- Irritation from hygiene products (bubble baths, scented wipes)
Quick reminder table:
| Cause | Clues it’s not an STD |
| Yeast infection | Thick white discharge, itching |
| Bacterial vaginosis | Odor, thin gray discharge |
| Hormonal changes | Dryness, skin changes |
| Soap/chemical irritation | Burning only after use of product |
👉 Personal note: I once heard from a friend who thought she had an STD after a beach trip. Turned out it was just a yeast infection flaring after wearing a damp swimsuit too long. Uncomfortable? Absolutely. Dangerous? Not really — but it sure felt scary at the time.
So yes, female urethra burning no std is more common than most people think, and it doesn’t always mean something’s seriously wrong. But if the burning lingers or pairs with unusual discharge or pelvic pain, a quick exam (and maybe a urine test) can save a lot of stress.
Alright — I’ll keep the rhythm going: conversational tone, weaving in burning tip of urethra no std and related semantic terms (personal care products, interstitial cystitis, urethral syndrome, bladder inflammation, etc.). I’ll also use a list, table, and a pro tip naturally.
7. Chemical Irritants & Personal Care Products
Sometimes the reason for a burning tip of urethra no std is as ordinary as your soap. Seriously. The urethra is delicate, and products we use every day — from bubble baths to laundry detergents — can trigger urethral pain without any infection behind it.
Common culprits include:
- Soaps and shower gels (especially perfumed ones)
- Bubble baths or bath bombs with dyes and glitter
- Lubricants or spermicide gels (some people are sensitive to chemicals like nonoxynol-9)
- Condoms (latex allergies can cause burning + skin changes)
- Laundry detergents or fabric softeners left in underwear
Some folks even react to barrier methods of contraception like diaphragms or condoms coated with spermicide. The irritation feels almost identical to a urinary tract infection, but urine tests or dipsticks show nothing.
Quick check Table:
| Irritant | How to Tell It’s the Cause |
| Soap/shower gel | Burning starts after shower or bath |
| Lubricant | Discomfort after sex, no other symptoms |
| Latex condom | Burning + redness/itching |
| Laundry detergent | Symptoms improve with unscented detergents |
👉 Pro tip: If the burning comes and goes, pay attention to your products. Switching to fragrance-free, hypoallergenic versions can sometimes solve the mystery overnight.
8. Overactive Bladder & Interstitial Cystitis
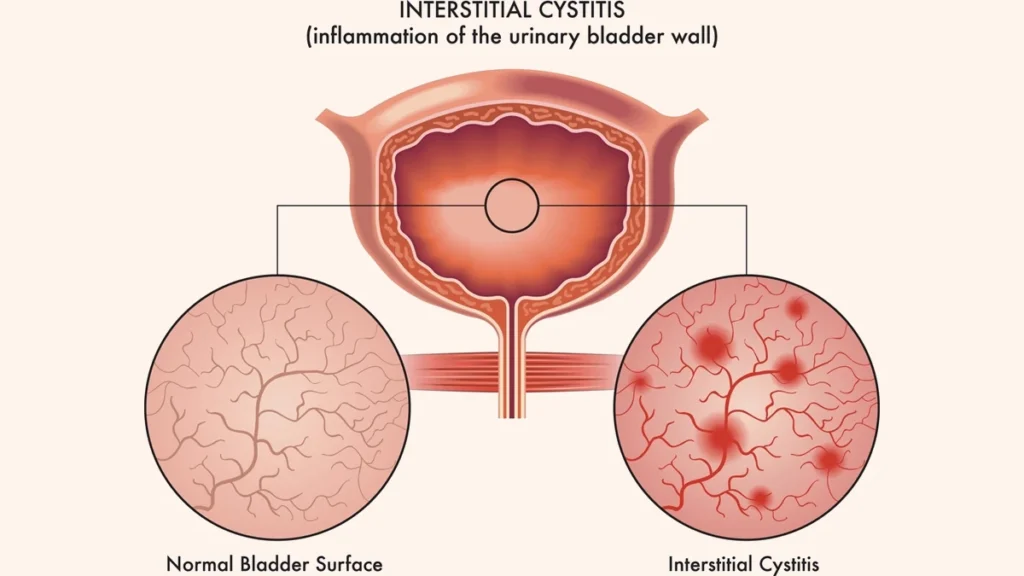
Not everything shows up on lab tests, and interstitial cystitis (IC) is a perfect example. Sometimes called painful bladder syndrome, it’s a chronic condition where the bladder lining gets irritated. That irritation spreads down into the urethra, leading to the same burning sensation people often mistake for an infection.
Symptoms usually include:
- Frequent urge to urinate (sometimes 40+ times a day in severe cases)
- Pelvic pain or pressure
- Burning at the urethra tip, especially after peeing
- Discomfort that worsens with certain foods (coffee, citrus, spicy dishes)
Doctors may use tools like a pelvic ultrasound, cystoscopy, or even a bladder biopsy to rule out other problems like bladder cancer. There isn’t a single cure, but treatments range from lifestyle changes (avoiding trigger foods, bladder training exercises) to prescription medications, and in some cases, physical therapy for pelvic floor muscles.
Foods that can flare IC symptoms (avoid if possible):
- Coffee or black tea
- Soda or alcohol
- Tomato-based sauces
- Citrus fruits
- Spicy foods
Foods that are bladder-friendly (usually safe):
- Pears, blueberries, melons
- Rice, oats, potatoes
- Chamomile tea
- Lean proteins (chicken, fish)
👉 Personal side note: A friend once thought they had endless UTIs, but urine cultures kept coming back negative. Eventually, a specialist explained it was IC. Tough at first, but with diet tweaks and bladder training, the burning and pelvic pain got so much better.
So yes — if the burning tip of your urethra lingers without clear signs of infection, urethral syndrome, or interstitial cystitis may be the missing piece.
9. Diabetes and High Blood Sugar
Another sneaky reason for a burning tip of urethra no std? Diabetes. When blood sugar runs high, extra glucose spills into the urine. That sugar-rich urine can irritate the lining of your bladder and urethra, making every bathroom trip feel sharp and uncomfortable.
But it’s not just the irritation — high blood sugar also creates a perfect environment for yeast overgrowth and bacteria, which increases your risk of urinary tract infections and bladder inflammation.
Clues that diabetes or high blood sugar may be playing a role:
- You’re peeing more than usual (polyuria)
- Feeling thirsty all the time
- Urine feels “sticky” or has a stronger odor
- Burning paired with fatigue or blurred vision
Doctors usually check this with a simple urine dipstick, blood sugar tests, or HbA1c levels. Managing diabetes doesn’t just protect your kidneys and nerves; it often eases urinary symptoms too.
Quick comparison:
| High Blood Sugar Effect | How It Shows Up in Urinary Symptoms |
| Sugar in urine | Burning, frequent urination |
| Weakened immune system | More UTIs |
| Nerve damage (long-term) | Bladder emptying issues |
| Yeast overgrowth | Irritation, itching |
👉 Pro tip: If you notice frequent burning without obvious infection, ask your doctor about blood sugar testing. Sometimes the bladder is the first place diabetes symptoms show up.
10. Medication Side Effects
Sometimes it’s not your body — it’s the meds. A surprising number of prescription drugs can make you feel like you’ve got a urinary infection when you don’t. That burning tip of urethra no std sensation is often listed under the “rare but possible” side effects in the fine print.
Common offenders include:
- Antibiotics (ironically, while they treat infections, they can also alter your natural balance and irritate tissues)
- Diuretics (water pills — they make you pee more often, which can dry and irritate the tract)
- Chemotherapy agents (some can inflame the bladder lining, known as hemorrhagic cystitis)
- Certain antivirals or antifungals (occasionally cause urethral irritation)
Doctors usually catch this pattern by ruling out infections with urine tests, urine cultures, or even nucleic acid amplification testing if they suspect nongonococcal urethritis, but nothing shows up. If your symptoms line up with the start of a new prescription, the timing can be a clue.
Table: Medications vs. Their Urinary Side Effects
| Medication Type | Possible Urinary Effect |
| Antibiotics (sulfa drugs) | Burning, altered urine odor |
| Diuretics | Frequent urination, dryness |
| Chemotherapy agents | Bladder inflammation, bleeding |
| Antivirals | Irritation, urethral pain |
👉 Pro tip: Don’t stop a prescribed medication on your own. If you suspect your meds are behind the burning, talk to your healthcare provider. Sometimes a switch, dosage adjustment, or pairing it with extra hydration makes all the difference.
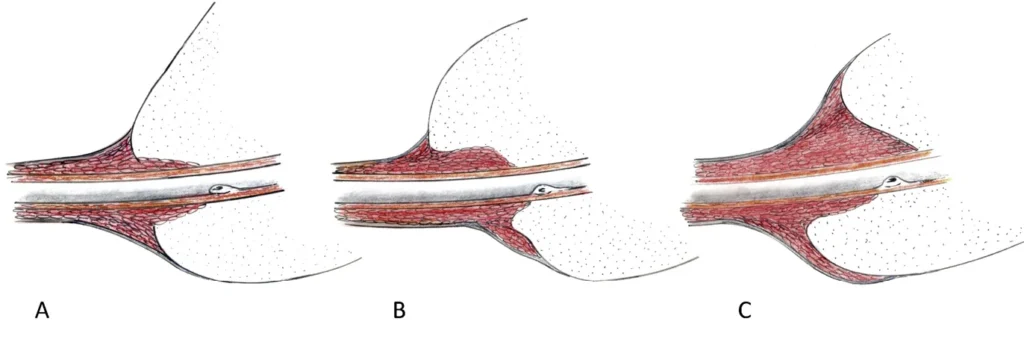
11. Recent Catheter Use or Medical Procedures

Sometimes the discomfort comes down to plain old trauma. If you’ve had a catheter, cystoscopy, or even certain surgeries, that burning tip of urethra no std sensation can just be your body healing. The urethra is a narrow, sensitive tube, and anything inserted (even for medical reasons) can cause micro-tears or inflammation.
Common procedures that may leave temporary burning:
- Urinary catheter placement (for surgery or bladder drainage)
- Cystoscopy (camera scope to check the bladder and urethra)
- Retrograde pyelogram (contrast dye imaging of the urinary tract)
- Hypospadias repair or prostate procedures
Usually, the pain eases within days to weeks, but sometimes infections can develop afterward — so if burning doesn’t improve, doctors might run urine cultures or imaging like an MRI of the pelvis.
Quick table of expected vs. concerning symptoms after procedures:
| Normal (healing) | Concerning (see doctor) |
| Mild burning when peeing | Fever, chills, worsening pain |
| Slight blood in urine | Heavy bleeding or clots |
| Increased frequency | Inability to urinate |
| Discomfort improving daily | Symptoms worsening after 3–4 days |
👉 Pro tip: Drink plenty of fluids post-procedure — it helps flush the urinary tract and shortens the irritation period. Some doctors also recommend mild pain relievers or urinary alkalinizers (like calcium glycerophosphate) to reduce stinging.
12. Sexual Activity & Physical Irritation
Not every urethral burn is a disease — sometimes it’s friction. Vigorous sex, prolonged masturbation, or even certain sex toys can leave you with a temporary burning sensation in the urethra. That burning tip of the urethra no std feeling often comes from tiny microtears or swelling around the opening.
When sexual activity might trigger urethral irritation:
- Rough or prolonged sex without enough lubrication
- Barrier methods of contraception (condoms with spermicide, or latex allergies)
- New lubricants or sex toys with harsh chemicals
- Post-sex dehydration (urine is concentrated, making it sting more)
Prevention tips:
- Always use adequate lubrication
- Pee after sex to flush out bacteria
- Stay hydrated before and after intimacy
- Choose hypoallergenic products if you’re sensitive
Small reflection: I remember a friend once panicked after a weekend getaway because he felt urethral pain every time he urinated. Turned out nothing was “wrong” — just a mix of dehydration, lots of intimacy, and a poor choice of overly perfumed lube. A few days of rest, water, and avoiding irritants made the burning fade.
Quick comparison list: Burning from irritation vs. STD infection
- Irritation: no discharge, clears in a couple of days
- STD: often paired with discharge, persistent pain, or systemic symptoms (fever, swollen lymph nodes)
👉 Pro tip: If the discomfort fades with hydration and rest, it’s probably irritation. But if burning lingers more than a few days, don’t guess — get tested. Urethral burning can mimic STIs, and only lab tests (like nucleic acid amplification testing) can rule them out completely.
13. Allergic Reactions (Latex, Lubricants, Medications)
Sometimes what feels like an infection is really your immune system overreacting. Allergic reactions in the genital area can cause redness, itching, and, yes, that burning tip of the urethra no std feeling. Doctors sometimes call this allergic urethritis, though it’s really irritation driven by hypersensitivity.
Possible triggers:
- Latex condoms (a surprisingly common allergy)
- Lubricants with fragrances, parabens, or glycerin
- Medications (topical creams, spermicides, and even some oral drugs)
- Personal care products (feminine sprays, scented wipes)
How to tell if it’s allergy-related?
- Burning or itching happens almost immediately after exposure
- Skin undertone changes — redness, swelling, or even a mild rash
- No systemic symptoms like fever (which infections often cause)
- Symptoms improve quickly once you avoid the trigger
Quick comparison table:
| Allergic Urethritis | Infection (UTI/STD) |
| Burning + redness right after product use | Burning develops over days |
| No fever, no discharge | May include discharge, fever, pelvic pain |
| Improves when the trigger is avoided | Persists until treated with antibiotics |
| Linked to specific product (condom, lube) | Linked to bacteria/viruses |
👉 Pro tip: If you suspect latex, try non-latex condoms (polyurethane or polyisoprene). For lubricants, stick with water-based, unscented, hypoallergenic options. Sometimes just one simple swap solves months of irritation.
14. Anxiety and Stress-Related Causes
Here’s something most people don’t expect: your mind can affect your bladder and urethra. Stress and anxiety can tighten pelvic floor muscles, amplify pain signals, and make the urethra feel like it’s burning — even without infection.
People with high stress often report urinary symptoms like:
- Needing to pee frequently (overactive bladder-type behavior)
- Burning sensation at the urethra, especially during high-anxiety days
- Pelvic pain or muscle tension that feels like an infection but isn’t
This is sometimes referred to as a psychosomatic contribution, where stress makes your body perceive pain more strongly. It doesn’t mean the symptoms are “in your head.” They’re real. The nerves in your bladder and pelvis are sensitive, and anxiety ramps them up.
Stress vs. Infection Clues:
| Stress-Related Burning | Infection-Related Burning |
| Comes and goes with stress levels | Persists regardless of stress |
| No discharge, no fever | Often, other systemic symptoms |
| Improves with relaxation techniques | Needs medical treatment |
| May pair with IBS, headaches, and muscle tension | Usually isolated to the urinary tract |
👉 Pro Tip: Techniques like pelvic floor relaxation exercises, mindfulness, or even talking to a health professional about stress can reduce burning sensations. A multidisciplinary approach — urologist + therapist — often helps when no infection explains the pain.
15. Rare Conditions (Cancer, Autoimmune Diseases, Nerve Issues)
Most of the time, that burning tip of urethra no std sensation comes from everyday things — dehydration, mild infections, or irritation. But once in a while, it signals something more serious. Rare conditions like urethral cancer, bladder cancer, or even penile cancer can present with persistent burning.
It’s not just cancer, though. Autoimmune diseases (like lupus or Sjögren’s syndrome) and nerve disorders (multiple sclerosis, diabetic neuropathy) can disrupt bladder function and trigger urinary symptoms. Even benign growths, like benign prostatic hyperplasia, may pinch the urethra enough to cause ongoing burning.
Red flag symptoms to never ignore:
- Blood in urine without a clear cause
- Unexplained weight loss + persistent urinary pain
- Skin changes around the genital area
- Burning that lasts weeks despite normal urine tests
Doctors may use a CT scan, MRI of the pelvis, retrograde pyelogram, or cystoscopy to investigate. Organizations like the American Cancer Society and clinical references (like Campbell Walsh Wein Handbook of Urology or Merck Manual Professional Version) stress that while rare, these causes must be ruled out when symptoms persist.
Quick table of rare but serious causes:
| Rare Condition | Possible Clues |
| Urethral or bladder cancer | Blood in urine, skin changes, pelvic pain |
| Autoimmune disorders | Burning + joint pain, fatigue |
| Nerve issues (MS, diabetic neuropathy) | Urinary urgency, incomplete bladder emptying |
| Penile cancer | Visible skin changes, swelling, and urethral pain |
👉 Pro Tip: If burning doesn’t improve after common causes are excluded, don’t delay. Ask your doctor for imaging or a specialist referral. Early diagnosis matters, and patient-centered care with a multidisciplinary approach (urologist, oncologist, neurologist) can make all the difference.
Conclusion
So, what’s the takeaway? A burning tip of urethra no std doesn’t always point to sexually transmitted diseases. From something as simple as dehydration or a reaction to selfcare products, to more complex issues like interstitial cystitis, prostatitis, or even rare cancers — there are plenty of possible explanations.
The key is figuring out patterns: does it flare after sex, during high stress, only when you’re dehydrated, or does it linger no matter what? Keeping track helps your healthcare provider narrow down causes.
A few self-care reminders:
- Stay hydrated (plain water is underrated)
- Use fragrance-free, hypoallergenic personal care products
- Don’t ignore persistent symptoms — urine tests and cultures matter
- Seek a professional opinion if burning lasts more than a few days or pairs with red-flag signs like blood in urine
And maybe most importantly, don’t spiral into worst-case scenarios too quickly. Yes, rare conditions exist, but most cases of urethral burning resolve with simple lifestyle changes, prescription antibiotics, or adjustments guided by a trusted health professional.
(Content disclaimer: This article is for informational purposes only and not a substitute for medical advice. Always consult your doctor or a qualified provider if you’re worried about urinary symptoms.)
People Also Ask (FAQ’s)
1. Why does my urethra burn but no infection?
A burning urethra without infection may come from dehydration, concentrated urine, friction, or bladder irritation. Conditions like interstitial cystitis or pelvic floor tension can also mimic infection-like symptoms.
2. How do I stop my tip from burning?
Drink plenty of water, avoid acidic or spicy foods, and use mild soaps to prevent chemical irritation. If burning continues, consult a doctor for tests to rule out hidden causes.
3. How do you fix a burning urethra?
Relief often comes from hydration, diet adjustments, and rest from irritants like cycling or rough activity. Persistent burning usually requires medical treatment such as antibiotics, anti-inflammatories, or lifestyle therapy.
4. Can you have an inflamed urethra without an STD?
Yes, inflammation of the urethra can occur from allergies, friction, or urinary issues such as kidney stones. Not all cases are linked to sexually transmitted infections.
5. Can masturbation cause urethritis?
Rough or excessive masturbation may cause temporary irritation and burning at the urethral tip. However, true urethritis usually stems from bacterial infection, not self-stimulation alone.
6. How do doctors test for urethritis?
Doctors typically order urine tests, swabs, or nucleic acid amplification testing (NAAT) to detect infection. In chronic cases, cystoscopy or pelvic imaging may be used for further evaluation.
7. How do you know if it’s a friction burn or STD?
Friction burns often improve within a few days with rest, hydration, and gentle care. STDs tend to cause persistent burning, discharge, or swelling—testing is the only way to confirm.
8. Does urethritis go away on its own?
Mild irritation may fade with time, hydration, and rest. But if urethritis is caused by bacteria or another medical condition, it usually worsens without professional treatment.
9. Could an infection cause a burning sensation?
Yes, urinary tract infections, prostatitis, and kidney infections commonly trigger urethral burning. A urine culture or lab test is needed to confirm and treat the infection properly.
10. When should I worry about a burning sensation?
You should worry if the burning lasts more than a few days, is severe, or comes with blood in urine, fever, or difficulty urinating. These signs need prompt medical evaluation.



