It’s a heavy question — how long before a pulmonary embolism kills you — but it’s the kind of thing people ask when they’re scared, or maybe just trying to make sense of something that feels invisible until it isn’t. A pulmonary embolism, or PE, can go from being this quiet, hidden threat to a full-blown medical crisis in a matter of minutes. And that’s the unsettling part: time really matters.
At its core, a pulmonary embolism happens when a blood clot makes its way into the lungs and blocks blood flow. Sometimes it’s small, and you get warning signs like shortness of breath or chest pain. Other times it’s massive, and — honestly — outcomes can turn fatal before anyone realizes what’s happening. That’s why timing isn’t just medical jargon here; it’s survival.
Still, it’s not all doom. With fast medical attention, treatments, awareness, and attitude matters for fitness survival chances improve a lot. The American Lung Association and the National Heart, Lung, and Blood Institute both emphasize that early recognition is half the battle. Which makes this conversation less about fear and more about being prepared.
What Is a Pulmonary Embolism?
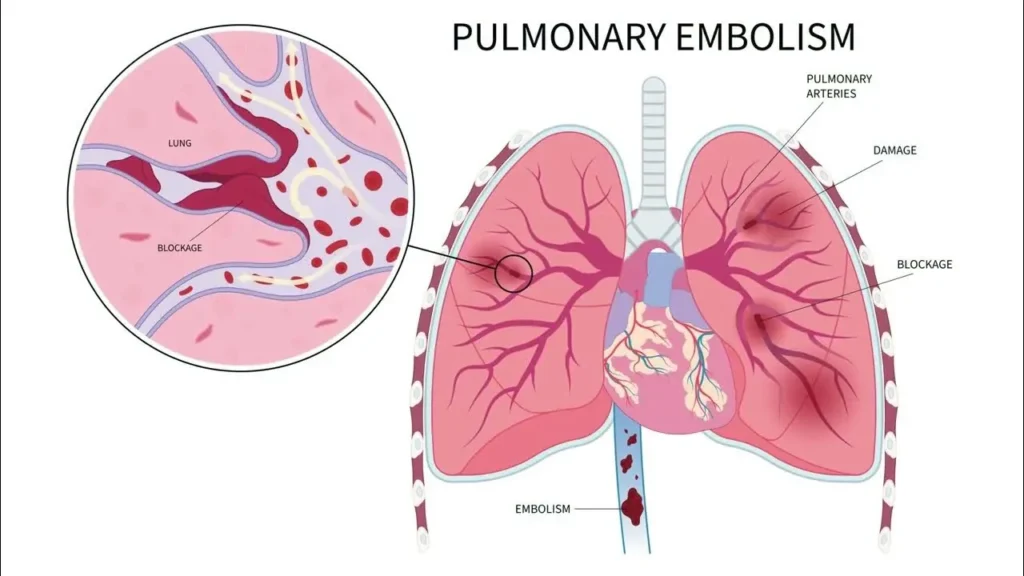
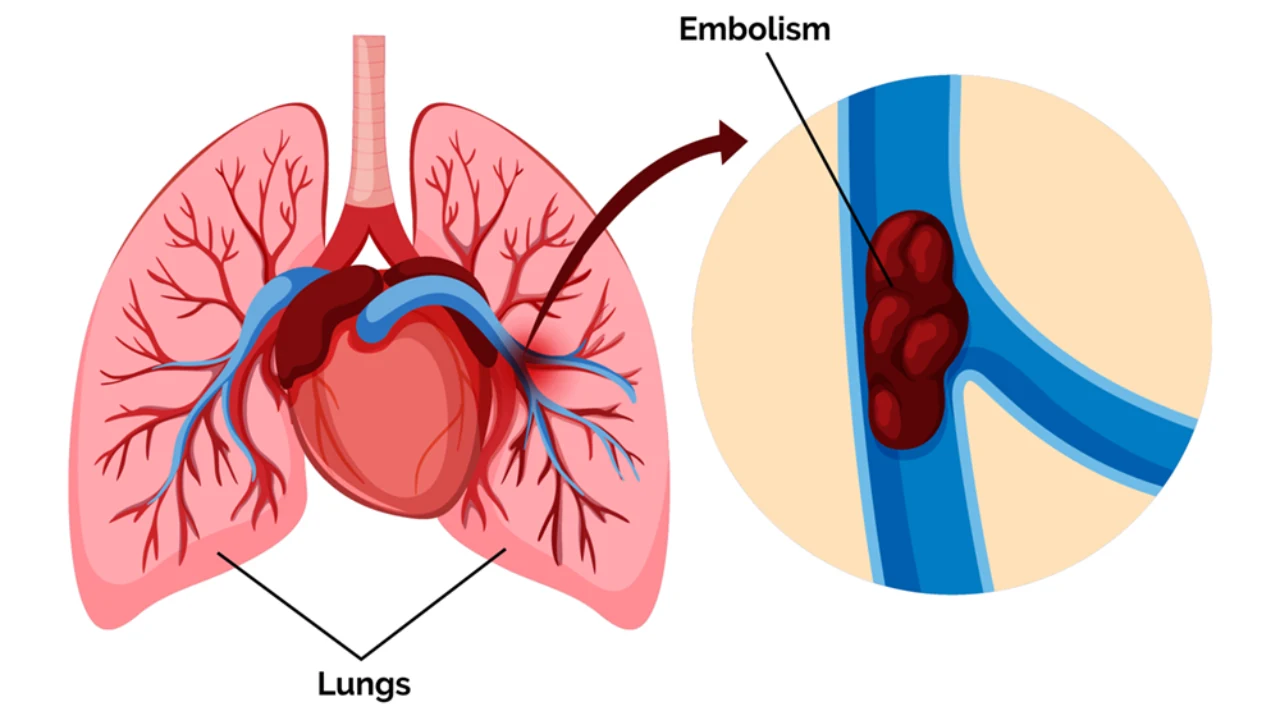
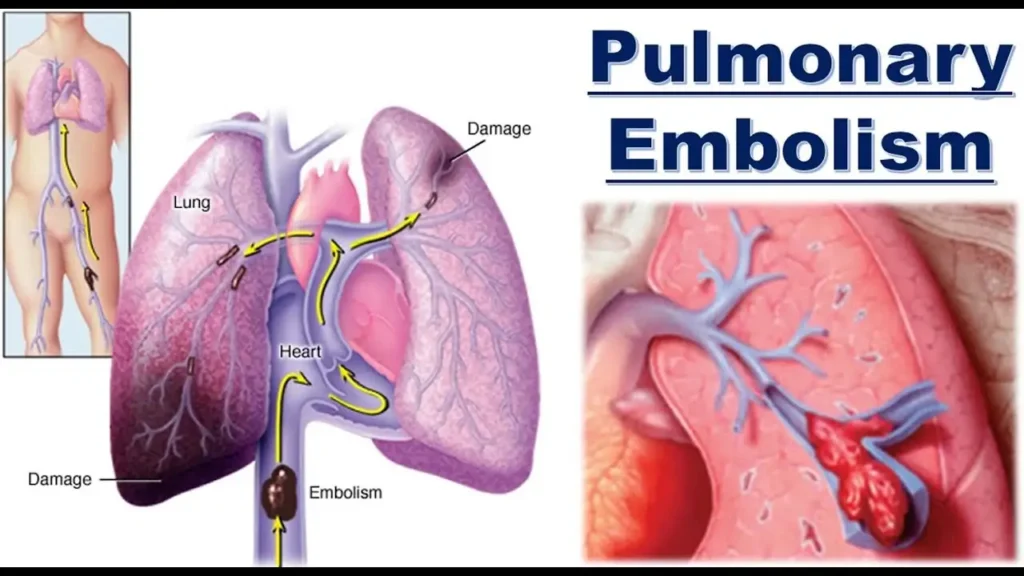
A pulmonary embolism (PE) is basically a blockage in one of the pulmonary arteries of your lungs. Most of the time, that blockage comes from a blood clot — usually one that forms in the legs (a condition called deep vein thrombosis, or DVT) and then breaks loose.
Imagine a small clot traveling like an unwanted passenger through your bloodstream until it wedges itself in a lung blood vessel. Suddenly, the flow is cut off.
The causes? Well, there are several:
- Prolonged immobility — long flights, bed rest, or even just too many hours sitting still.
- Surgery or injury — because recovery periods slow circulation and raise clotting risks.
- Cancer and certain medical conditions — some diseases make clotting more likely.
- Lifestyle factors — smoking, obesity, or dehydration can all increase risks.
And while this sounds like a medical textbook, think of it more like a chain reaction. One small clot in your leg can cause this cascading problem that ends up in the lungs, creating an emergency situation.
Who Is at Risk?
Here’s where it gets personal. Pulmonary embolism doesn’t just appear out of nowhere — there are high-risk groups that face it more often:
- Older adults with slower circulation.
- Pregnant women, since blood volume and clotting factors change.
- People with clotting disorders.
- Anyone with a sedentary lifestyle — think desk jobs, long-haul travel, or recovery from surgery.
And then there’s the simple question people often ask: how does a blood clot actually travel to the lungs? The answer is surprisingly straightforward — the clot forms in a deep vein (often in the leg), dislodges, and gets carried by the bloodstream through the veins, into the right side of the heart, and then straight into the pulmonary arteries. That’s the “moment” when it turns from a leg problem into a lung problem.
How Fast Can a Pulmonary Embolism Kill You?
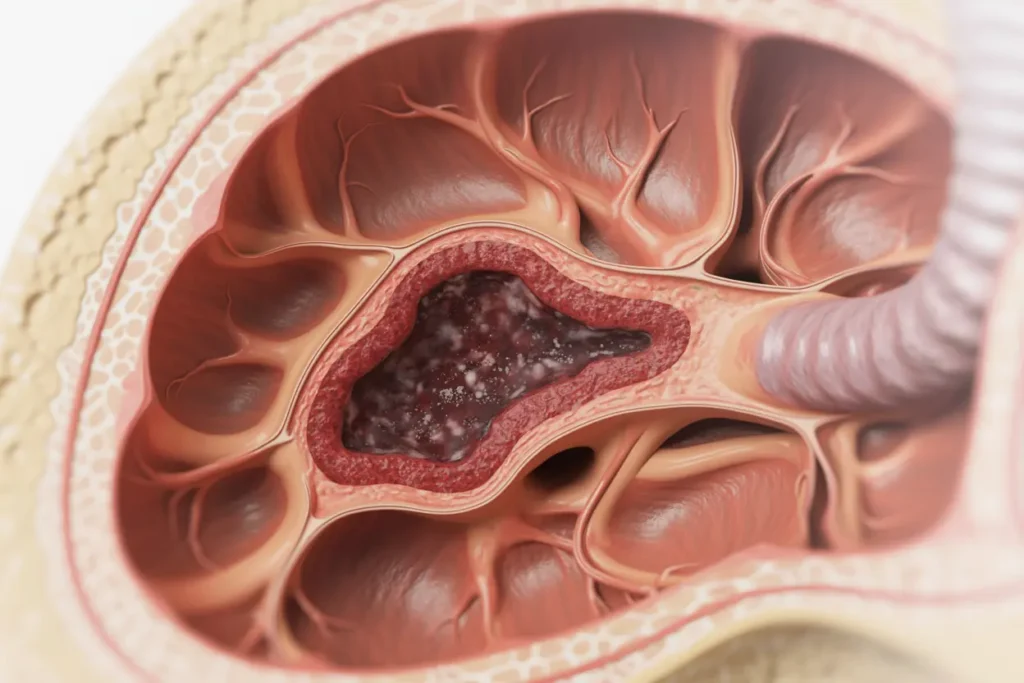
It’s a blunt question — how long before a pulmonary embolism kills you — and the uncomfortable truth is: sometimes, it’s very quick. When a clot blocks a major blood vessel in the lungs, oxygen flow plummets, the heart strains to pump against the blockage, and collapse can happen within minutes.
Cases reported in JAMA Netw Open 2020;3(8):e2010779 show that massive pulmonary embolism can cause sudden death before emergency care is even reached.
But here’s the nuance: not every PE acts the same way.
- Sudden Onset: A massive clot can overwhelm the system almost instantly.
- Gradual Progression: Smaller clots may cause chest pain, shortness of breath, or coughing up blood before escalating.
A lot depends on the size and location of the clot, as well as underlyi \ng medical conditions like heart disease, obesity, or cancer. The American Heart Association notes that with prompt treatment — blood thinners, clot-busting drugs — survival improves dramatically.
Survival Timeline Statistics
To put it into perspective, here’s how survival looks based on timing:
| Time After Onset | Risk of Death | Notes |
| Within 1 hour | Very high (massive PE can be instantly fatal) | Sudden collapse common |
| First 24 hours | Mortality drops with urgent treatment | Most deaths occur if untreated |
| First week | Stabilization is possible with anticoagulants | Risk of recurrence if untreated |
| Beyond 30 days | Most patients recover, though some develop chronic issues | Monitoring essential |
So, can someone survive a pulmonary embolism without treatment? Honestly — the risk of death skyrockets.
While there are rare stories of survival, studies like those by Barnes GD, Muzikansky A, Cameron S, Silva MJ, Mendes C point out that untreated PEs often lead to sudden collapse or progressive respiratory failure.
In other words, without medical attention, survival is the exception, not the rule.
Symptoms That Signal Immediate Danger
Pulmonary embolism is tricky because its symptoms can either scream “emergency” or whisper so softly they’re mistaken for anxiety or the flu. Knowing what to watch for can literally save your life.
Common Warning Signs
- Shortness of breath — even when sitting still.
- Chest pain — sharp, stabbing, worse when breathing deeply.
- Rapid heartbeat — sometimes racing for no clear reason.
- Coughing up blood — a serious red flag that blood flow is blocked.
These symptoms don’t mean you always have a PE, but when they appear suddenly — especially together — the risk of a blood clot becomes a genuine emergency.
Silent Symptoms
Here’s the scary part: not every pulmonary embolism makes itself obvious. Some people experience vague fatigue, lightheadedness, or mild chest discomfort that gets brushed off. Others are misdiagnosed with pneumonia, asthma, or even a panic attack.
Research in Cardiovasc Diagn and Libyan J Med highlights how silent or misinterpreted symptoms delay treatment, raising the risk of death.
Pro Tip: If you’re someone with medical conditions like prior DVT, heart disease, or cancer, don’t ignore even mild symptoms. The Centers for Disease Control and Prevention (CDC) stresses that early testing (like CT scans or D-dimer blood tests) in the emergency department can catch clots before they become fatal.
Emergency Response: What to Do If You Suspect a PE
So, what do you actually do if you think you — or someone near you — might be having a pulmonary embolism? Well, the first and most important thing is: don’t wait it out.
The whole idea of how long before a pulmonary embolism kills you comes down to this window of time where medical attention changes everything.
First Aid and Urgent Care
If symptoms hit suddenly (shortness of breath, chest pain, coughing up blood), call emergency services immediately. No hesitation, no “let’s just see if it passes.” Every minute counts when blood flow is blocked.
What to do while waiting for help:
- Keep the person calm and sitting upright — lying flat can worsen breathing.
- Avoid giving aspirin or over-the-counter meds unless directed by medical staff.
- Be ready to share health history (DVT, recent surgery, cancer, pregnancy, clotting disorders).
Hospital Treatment Protocols
Once you’re in the emergency department, things move quickly. Doctors use imaging techniques (such as CT, pulmonary angiography, and ventilation-perfusion scans) and blood work to confirm the presence of a clot. Treatment depends on clot size, blood test and overall stability:
- Oxygen therapy to support breathing.
- Anticoagulants (blood thinners) like heparin or warfarin are used to stop further clotting.
- Thrombolytics (clot-busting drugs) for massive PE cases — risky but life-saving.
- Surgical procedures like catheter-directed clot removal or embolectomy when drugs aren’t enough.
Research from Hsu SH, Ko CH, Chou EH, Herrala J, Wang CH, Chang WT, Huang CH, Tsai CL emphasizes that rapid intervention reduces the death rate dramatically, especially when clot-busting therapy is given within hours of symptom onset.
Pro Tip: Always mention recent travel, surgery, or prolonged immobility to the ER staff. That detail helps doctors zero in on PE faster and may literally save your life.
Factors That Influence Survival Time
Why do some people collapse within minutes, while others survive long enough to get treated? The answer isn’t just the clot — it’s a mix of clot characteristics and your personal health background.
Size and Location of the Clot
- Massive PE: A large clot blocks the main pulmonary artery. This can stop blood flow instantly, leading to sudden cardiac arrest.
- Submassive PE: Smaller clots in medium vessels — serious but with a higher chance of survival if treated quickly.
- Peripheral PE: Small, scattered clots in the outer branches. Painful, scary, but often manageable with anticoagulants.
Doctors often explain it as “real estate matters.” A clot in a central lung vessel cuts off oxygen fast, while smaller clots give more time to act.
Underlying Health Conditions
Your body’s baseline health matters too. Conditions like:
- Heart disease — puts extra strain on circulation.
- Obesity — slows blood return and increases clotting risk.
- Cancer — especially active cancers, which change clotting factors.
- Prior DVT or clotting disorders — make recurrence more likely.
Studies cited by Ibrahim WH, Hussein MS, Kamel A, Abu Afifeh LM, Karuppasamy G and others show survival odds drop sharply when PE overlaps with serious chronic disease.
Pro Tip: If you fall into a high-risk group, consider preventive strategies — compression stockings, staying hydrated, moving frequently on long trips — because the risk of blood clot formation isn’t theoretical. Prevention is easier than surviving a medical emergency.
Long-Term Survival and Recurrence
Here’s the thing: surviving the initial event doesn’t mean the story ends. People often wonder, How long before a pulmonary embolism kills you if it happens again? And that’s a fair concern, because once you’ve had a PE, the risk of recurrence is higher than average.
Recovery Outlook
Most people do recover — especially with rapid treatment. According to the American Lung Association and the National Heart, Lung, and Blood Institute, anticoagulant therapy lowers recurrence risk significantly.
But recovery isn’t just medical; it’s also about lifestyle. You might find yourself rethinking long flights, desk hours, or even how often you stretch your legs.
What to expect after recovery:
- Fatigue and mild chest discomfort can linger for weeks.
- Follow-up scans and blood work are standard.
- Lifestyle adjustments (exercise, diet, hydration) play a huge role in preventing another clot.
Risk of Recurrence
The scary part is recurrence, which isn’t rare. Studies like those by Kay FU, Wolosker N, Bach AG, Taute BM, Meyer HJ, Schramm D show that without continued anticoagulation, clots can re-form within months.
| Risk Factor | Chance of Recurrence | Notes |
| Stopping anticoagulants early | High | Especially in the first 6–12 months |
| Active cancer | Very high | Cancer alters clotting pathways |
| Genetic clotting disorders | Moderate to high | Lifelong monitoring often required |
| Lifestyle factors (smoking, immobility) | Moderate | Preventable with changes |
Pro Tip: Even if you feel fine, never stop medication without medical clearance. The risk of death from recurrent PE is higher than the first event because people underestimate it.
Prevention: Reducing Your Risk of a Fatal PE
The blunt answer to how long before a pulmonary embolism kills you often comes down to prevention. If you stop the clot before it reaches the lungs, you change the outcome entirely.
Lifestyle Changes
Simple adjustments lower the risk of blood clot formation dramatically:
- Stay active — walking breaks during work or travel.
- Hydrate — dehydration thickens blood, making clots more likely.
- Avoid smoking — it damages blood vessels and accelerates clotting.
- Stretch during flights or car rides longer than 4 hours.
Think of it less as “exercise for fitness” and more as “circulation maintenance.”
Medical Prevention
For high-risk individuals, doctors may recommend:
- Compression stockings to keep blood moving in the legs.
- Anticoagulants (long-term for some patients).
- Routine checkups with specialists, especially if you’ve had DVT or prior embolisms.
The Centers for Disease Control and Prevention (CDC) and American Heart Association both emphasize that these preventive strategies cut down not just clot formation, but also hospitalizations and long-term complications like chronic thromboembolic pulmonary hypertension.
Pro Tip for Travelers: Long flights? Set a timer to walk every 2 hours. If you can’t, at least do calf raises or ankle circles in your seat. It seems silly — but clots love stillness, and movement is your best defense.
Pulmonary Embolism vs. Other Emergencies
One of the confusing parts about how long before a pulmonary embolism kills you is that the symptoms often mimic other emergencies. Chest pain, dizziness, sudden shortness of breath — they can sound like a heart attack or even a stroke. Knowing the differences helps you (and doctors) act faster.
Comparison with Heart Attack and Stroke
Here’s a quick side-by-side look at how these emergencies overlap and differ:
| Condition | Main Cause | Common Symptoms | Urgency |
| Pulmonary Embolism (PE) | Blood clot blocking lung arteries | Shortness of breath, chest pain, coughing blood, rapid heartbeat | Can be fatal within minutes–hours |
| Heart Attack | Blockage in coronary artery | Crushing chest pain, pain radiating to arm/jaw, sweating, nausea | Fatal if not treated within hours |
| Stroke | Blockage or bleed in brain blood vessels | Slurred speech, weakness on one side, vision loss | Brain damage within minutes |
The American Heart Association points out that PE and heart attack both strain circulation but in different organs — the lungs vs. the heart. A heart attack feels like “pressure” in the chest, while a pulmonary embolism often feels like stabbing pain with every breath.
Pro Tip: If you can’t tell which one it is, don’t try to self-diagnose. In the emergency department, imaging and blood tests quickly separate heart disease from blood vessel disease in the lungs.
When to See a Doctor
You don’t have to wait until you’re gasping for breath to get checked. A lot of people ask, Should I see a doctor if I only suspect a clot? The answer is: yes, because the risk of blood clot formation often shows up with small warning signs first.
Routine Screening
If you’re high-risk (older age, history of DVT, bowel cancer, obesity, genetic clotting disorders), routine checkups make sense. The National Heart, Lung, and Blood Institute even suggests proactive imaging for patients with repeat clots.
Screenings might include:
- Ultrasound of the legs for DVT.
- Blood tests (D-dimer) for clot fragments.
- CT scans are performed if shortness of breath or chest pain is unexplained.
Early Medical Consultation
Even without a confirmed PE, there are times to see a doctor:
- Persistent leg swelling or pain (possible DVT).
- Sudden unexplained chest pain.
- Shortness of breath with light activity.
And here’s the subtle thing: sometimes, people ignore these because they chalk them up to anxiety or being out of shape. But research from Saboo SS, Tanabe Y, Landay MJ, Kay FU, Turetz M shows that early recognition and treatment of distant clots lowers the death rate significantly.
Pro Tip: If you’re recovering from surgery, traveling long-haul, or living with conditions like cancer or heart disease, make “when in doubt, check it out” your personal rule. Catching a clot early is the best way to avoid asking later how long before a pulmonary embolism kills you.
Conclusion
So, how long before a pulmonary embolism kills you? The truth is, it varies — sometimes minutes, sometimes hours, and in many cases not at all, if it’s caught in time. The difference between survival and tragedy usually comes down to awareness and action. Recognizing symptoms like shortness of breath, chest pain, or coughing up blood — and not brushing them off — buys you the time to get lifesaving treatment.
Medical research — from the American Heart Association to journals like JAMA Netw Open and Cardiovasc Diagn — keeps repeating the same message: speed matters. Blood clots don’t wait politely. But the good news is, prevention and prompt care work. Compression stockings, anticoagulants, staying active on long trips — these aren’t just small habits; they’re shields against what could otherwise be fatal.
In the end, maybe the better question isn’t how long before a pulmonary embolism kills you, but rather, how quickly can you recognize and respond? Because survival is not luck alone — it’s also awareness.
People Also Ask (Faq’s)
1. How long can a person live with blood clots in their lungs?
Some people live for days or weeks if the clot is small, but untreated pulmonary embolism can turn fatal quickly. Survival depends on early medical attention. With prompt treatment, many people go on to live normal, healthy lives.
2. What are the three stages of pulmonary embolism?
Doctors often describe them as mild (small clots with few symptoms), submassive (moderate blockage with strain), and massive (life-threatening with high death risk). The stage determines both the severity and urgency of treatment.
3. Is death from pulmonary embolism quick?
Yes, massive pulmonary embolism can cause sudden collapse within minutes. Smaller clots progress more slowly, giving a chance for treatment. This is why recognizing symptoms early is lifesaving.
4. Can you fully recover from a pulmonary embolism?
Many people recover completely with blood thinners and lifestyle changes. Some may develop long-term lung or heart complications if the clots are severe. Regular follow-up care helps lower this risk.
5. How long does it take for a blood clot to dissolve with blood thinners?
Blood thinners stop new clots from forming, but don’t “melt” old ones instantly. Clots often shrink naturally over weeks to months. The timeline varies based on clot size and overall health.
6. What is the main cause of blood clots in the lungs?
Most clots start in the legs as deep vein thrombosis (DVT). They break off, travel through the bloodstream, and lodge in the lung’s blood vessels. Risk factors include immobility, surgery, and certain medical conditions.
7. What is the red flag for pulmonary embolism?
Sudden shortness of breath with chest pain or coughing up blood is the biggest warning. A rapid heartbeat is another serious red flag. If these occur, emergency care is critical.
8. What is considered a large PE?
A massive PE is when a clot blocks the main pulmonary artery or both lungs’ major vessels. These are highly fatal without immediate treatment. Such cases often require advanced interventions like clot-busting drugs
9. What are the five warning signs of a blood clot?
Swelling, warmth, redness, pain in the leg, and tenderness when standing or walking. These often point to DVT, the main source of lung clots. Recognizing them early can prevent a deadly embolism.
10. What is the mode of death in pulmonary embolism?
Most deaths happen due to sudden heart failure when blood flow is blocked. The body can’t deliver oxygen, leading to collapse. This highlights the urgent need for early diagnosis and therapy.
11. How fast does a blood clot travel from the leg to the lungs?
Once dislodged, it can reach the lungs in seconds through the bloodstream. That’s why sudden symptoms strike so quickly. Immediate medical help is the only safe response.