You glance down one day — maybe after lifting weights, or even just folding laundry — and suddenly notice something strange: sudden bulging veins in hands with pain. They weren’t like that yesterday, right? It’s an odd mix of fascination and worry. The veins look raised, maybe a little throbbing, and you can’t help but wonder what’s going on beneath your skin.
Sometimes it’s totally harmless — a simple response to heat, exercise, or just gravity doing its thing. Other times, though, those bulging veins are your body’s quiet way of asking for attention. Veins react to more than we realize: temperature, hydration, blood pressure, even stress. When blood flow changes or the one-way valves inside your veins weaken a little, the veins can puff up or feel tender.
It’s easy to jump to scary conclusions about blood clots test or varicose veins (and we’ll talk about those, don’t worry), but most of the time, these changes are your body adapting to small shifts — in circulation, activity, or even your posture. Still, if you’ve felt that pinch of pain or noticed veins that stay swollen longer than usual, it’s worth learning what your hands might be trying to tell you.
So, in this guide, we’ll unpack what’s normal and what’s not — from everyday triggers like dehydration and exercise to medical causes like vein inflammation or vascular disease. And maybe along the way, you’ll see your body not as a mystery to fix, but a story to listen to.
Understanding how sudden bulging veins in hands with pain

If you think about it, your veins are like the quiet roadways beneath the surface — busy, essential, and mostly ignored until traffic builds up. When you notice bulging veins in your hands or arms, what you’re really seeing is your body’s blood flow adapting.
It’s not just about looks; it’s a whole system at work, pushing deoxygenated blood back toward the heart against gravity.
1. How Blood Moves Through Veins: The Return Trip to the Heart
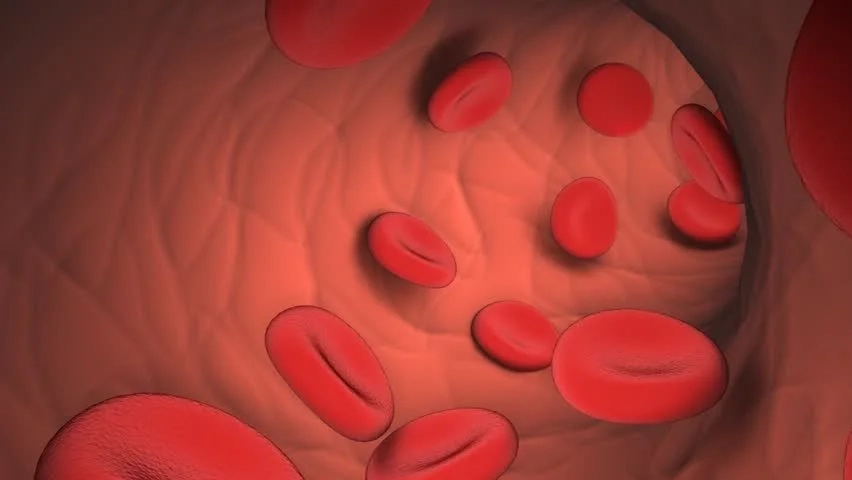
Unlike arteries, which carry blood away from the heart, veins are responsible for the uphill journey — a steady return trip through a network of superficial veins (close to the skin) and deep veins buried near your muscles. Inside them, tiny one-way valves open and close to keep blood flowing in the right direction. When those valves weaken — from aging, pressure, or injury — blood can pool, creating what you see as bulging or veiny hands.
This pooling isn’t always dangerous, but sometimes it hints at chronic venous insufficiency, a condition where blood struggles to return upward efficiently. It can also relate to varicose veins, vein inflammation, or even early signs of a vein disorder like superficial thrombophlebitis.
2. Why Veins Appear More Visible: Skin, Fat, and Hydration

Ever noticed your veins looking more pronounced after a workout or on a hot day? That’s not your imagination. Blood flow increases during physical activity, and heat causes veins to dilate so your body can release warmth.
In those moments, especially when subcutaneous fat is low or skin thickness decreases (like with aging), your veins stand out more.
Here’s a quick look at what influences that visibility:
| Factor | What Happens to Veins | Why It Matters |
| Intense exercise or cardio | Veins expand due to increased blood flow | Temporary — improves oxygen delivery |
| Hot weather or dehydration | Veins dilate to release heat | Often paired with mild swelling or vein tenderness |
| Low body fat or high muscle tone | Veins become more defined and raised | Common in athletes — often harmless |
| Aging or thinning skin | Less fat cushions superficial veins | Makes bulging veins more noticeable |
3. The Role of Valves and Pressure
Inside every vein are those small one-way valves that act like traffic lights, keeping blood pooling to a minimum. But when those valves start malfunctioning — maybe from high blood pressure, vascular diseases, or just wear and tear — blood can backflow, stretching the vein walls and causing that tender, rope-like bulge.
Over time, repeated strain on these valves may lead to superficial vein thrombosis or deep vein thrombosis (DVT) if clots form deeper in the arm or upper extremities. That’s why understanding these early visible signs is so important for vascular health — it’s your first clue that something inside might need attention.
🩸 Pro Tip: If your veins often pop after exercise and stay raised for hours with pain and tenderness, try gentle compression therapy or cooling the area with a damp towel. It helps reduce swelling and keeps the vein inflammation from worsening.
Common Causes of Sudden Bulging Veins in Hands with Pain
You know that moment when your hands suddenly look… different? The veins rise like tiny ridges under the skin, sometimes aching just enough to make you notice. That’s the thing about sudden bulging veins in hands with pain — they can appear for so many reasons, from the totally harmless to the quietly serious.
Some are as simple as an intense workout, while others involve deeper vascular issues or vein inflammation that your body can’t just shake off.
Let’s break down the most common reasons — and what each might be trying to tell you.
1. Intense Exercise or Weightlifting

When you’re lifting, sprinting, or doing blood flow resistance training, your veins expand to keep up with your muscles’ oxygen needs. This temporary blood pooling makes them stand out more, especially in the upper extremities. After the workout, they should slowly flatten as circulation normalizes.
🩸 Pro Tip: Alternate heavy lifting with lighter routines or stretching days. It supports vascular health and prevents overstraining vein valves that can lead to vein pain and swelling later on.
2. Heat or Dehydration
Hot weather or a steamy sauna session? Your body naturally dilates blood vessels to release heat. Combine that with mild dehydration, and the veins in your hands might appear more prominent and tender. This is because reduced blood volume makes veins stand out closer to the skin.
Quick tip: Keep fluids balanced — not just water but electrolytes too — since dehydration thickens the blood and can stress superficial veins unnecessarily.
3. Aging and Skin Changes

As we age, our subcutaneous fat layer thins and our vein walls lose elasticity. That means superficial veins become more visible and occasionally ache due to weakened vein valves. This process is normal, but in some cases, it can evolve into chronic venous insufficiency or varicose veins in the hands.
| Age-Related Change | Impact on Veins | Possible Outcome |
| Thinner skin | Makes veins appear closer to the surface | Cosmetic, often harmless |
| Weaker vein walls | Allows slight blood backflow | May cause bulging veins |
| Loss of fat & collagen | Less cushion for veins | Pain and tenderness after activity |
4. Stress and Blood Pressure Spikes

Ever notice how your body reacts when you’re anxious or tense? Stress hormones like adrenaline can raise blood pressure, temporarily straining blood vessels and making veins pop out, especially if your hands are clenched often. It’s not a major medical issue by itself, but chronic stress might lead to vascular disease or worsening vein inflammation.
5. Injury, Inflammation, or Infection
If you’ve ever bumped your hand or had a minor cut that became red, warm, or swollen — that’s your body’s inflammatory response at work. In some cases, though, this can turn into superficial thrombophlebitis, where a small clot forms in a superficial vein, causing localized pain and tenderness.
More severe forms, like deep vein thrombosis (DVT) in the arm, are rare but serious. You might feel the pain spread, or the area could look discolored. DVT sometimes links to venous thromboembolism, which can travel to the lungs and cause a pulmonary embolism — a true emergency.
6. Varicose or Spider Veins
These are probably the most misunderstood of all vein diseases. Varicose veins in the hands happen when vein valves fail to close properly, allowing blood to collect and push the vein outward. It’s less about appearance and more about blood flow resistance and vein wall weakness.
Spider veins are smaller, thread-like networks visible under the skin — often harmless, but they can indicate early vascular issues if accompanied by hand vein pain or vein inflammation.
🩸 Pro Tip: If your hand veins remain swollen, warm, or sore for days, consult a vein specialist or vascular surgeon. They might suggest diagnostic tools like ultrasound imaging or minimally invasive treatments such as Endovenous Laser Ablation or Radiofrequency Ablation. These methods target damaged veins without major surgery.
When to Worry: Warning Signs of Underlying Conditions
Most of the time, those raised, pulsing lines across your hands fade on their own — but sometimes, sudden bulging veins in hands with pain are more than just a quirk of circulation. They can signal deeper vascular issues, like a blood clot, vein inflammation, or even an early stage of chronic venous insufficiency. The trick is knowing when to brush it off… and when to pay attention.
There’s a fine line between what’s normal and what’s not. Below are a few red flags that your veins might be trying to warn you about.
1. Blood Clots (Thrombophlebitis)
A blood clot in a superficial vein — called superficial thrombophlebitis — can cause localized swelling, redness, and tenderness. It often feels like a firm cord under the skin. If the clot forms deeper, in a deep vein, that’s deep vein thrombosis (DVT) — a more serious condition that can cause pain and swelling in the entire arm or hand.
If left untreated, a DVT can lead to venous thromboembolism or even a pulmonary embolism, where the clot travels to the lungs and blocks blood flow — something you absolutely don’t want to ignore.
| Type of Clot | Location | Typical Symptoms | Severity Level |
| Superficial Thrombophlebitis | Near the skin’s surface | Redness, warmth, tenderness, visible lump | Mild to moderate |
| Deep Vein Thrombosis (DVT) | Deep within muscles or upper extremities | Swelling, intense pain, bluish skin tone | Serious – needs immediate medical care |
🩸 Pro Tip: If one hand suddenly swells, feels warmer, or looks discolored compared to the other, seek help immediately. Ultrasound examination or ultrasound imaging can quickly detect deep vein thrombosis before complications arise.
2. Venous Insufficiency
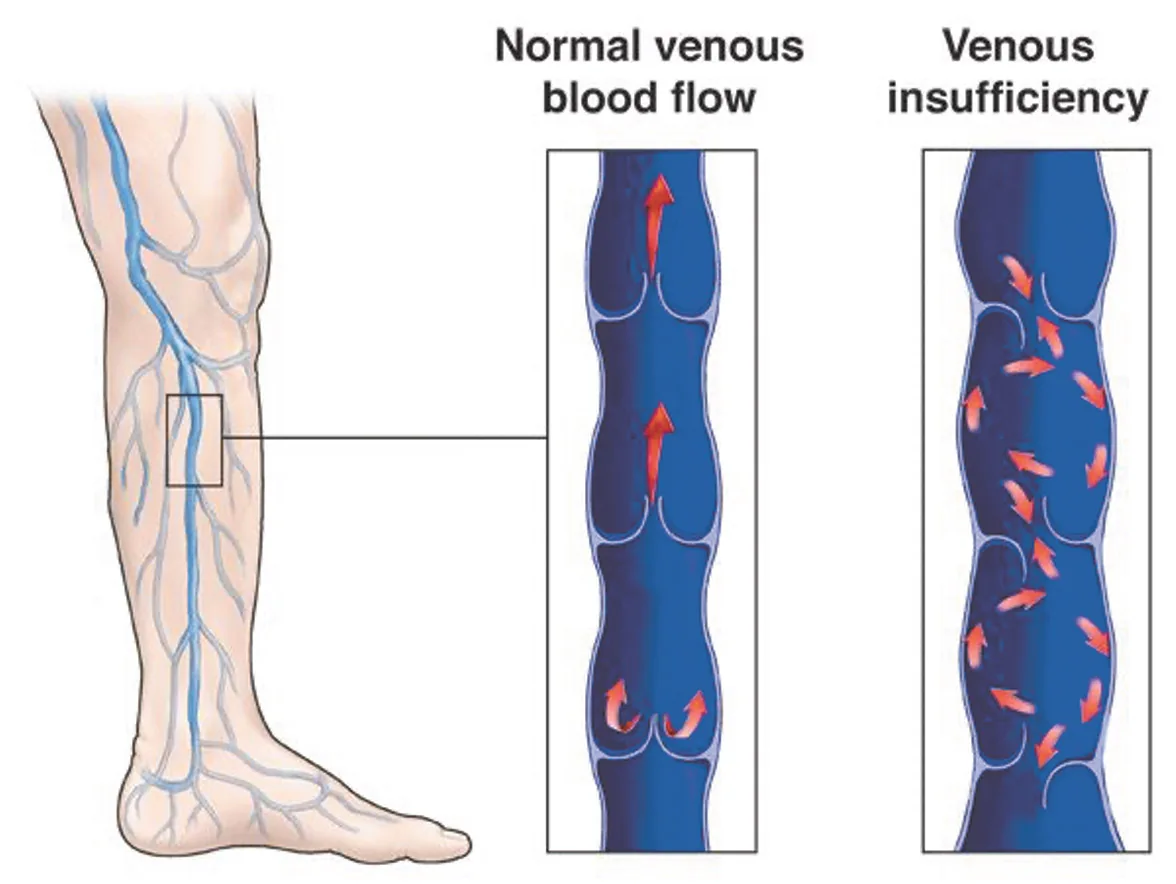
When vein valves don’t close properly, blood flows backward and starts pooling in the veins. Over time, that pressure weakens the vein walls, leading to swelling, heaviness, and sometimes visible varicose veins in your hands or forearms. This condition, known as chronic venous insufficiency, often gets worse when you stand or sit for long periods without moving.
You may also notice skin changes, small spider veins, or a feeling of muscle cramps in your hands or wrists, especially at night. It’s one of those slow-developing vein disorders that creeps up over months or years.
3. Vascular Disease
Not all vein pain and swelling start from clots. Sometimes, it’s a sign of broader vascular disease, where blood vessels narrow or stiffen due to plaque buildup or inflammation. That restriction limits blood flow, creating resistance that makes veins bulge and ache.
Conditions like peripheral vascular disease or aortic aneurysm (less common but dangerous) can cause similar sensations — tightness, tingling, or that dull ache you can’t quite explain. In autoimmune cases, such as Behçet’s disease, Giant cell arteritis, or temporal arteritis, the inflammation affects both arteries and veins, sometimes bringing head pain, jaw pain, or even vision problems into the picture.
4. Infection or Inflammation
Sometimes, the problem starts on the surface — a skin infection like cellulitis that spreads to nearby veins, causing pain, redness, or warmth. This can evolve into vein inflammation or, in rare cases, a vein trauma reaction after an IV line insertion.
Mild infections might resolve with anti-inflammatory medicines, but if the area feels hot to the touch or develops streaking redness, that’s a clear signal to see a vascular specialist.
🩸 Pro Tip: Don’t confuse temporary soreness from a workout with vascular inflammation. If your veins stay swollen or tender for more than 48 hours — or if pain worsens instead of easing — it’s worth getting a quick ultrasound test. Many clinics like the Center for Vein Restoration or Astra Vein Treatment Center offer non-invasive scanning tests that take less than 30 minutes.
Diagnosing the Cause: What a Doctor Might Check
If your hands still ache or those veins just won’t settle down, it’s time to look beyond guesswork. Diagnosing sudden bulging veins in hands with pain isn’t about rushing into scary conclusions — it’s about finding clarity. A good vascular specialist or vein doctor doesn’t just glance at your hands; they look at your whole vascular pattern, your history, and how your veins behave under different conditions.
You might be surprised how much your hands can reveal with the right tools — from ultrasound machines that track blood flow to blood tests that spot subtle signs of inflammation or autoimmune conditions.
1. Physical Exam & Medical History: When Your Hands Tell a Story
The first step is usually simple observation. Your doctor will ask when you noticed the bulging veins, whether the pain and tenderness come and go, and if you’ve had recent injuries, IV lines, or intense cardio exercise. They’ll also check for visible spider veins, vein inflammation, skin changes, or color differences between both hands.
Sometimes, just talking about your physical activity, hydration habits, or even emotional stress can reveal patterns — like how blood pressure spikes during anxiety or body fat loss from workouts makes veins more visible.
2. Imaging & Ultrasound Tests: Seeing Beneath the Skin

If your doctor suspects something more complex — like deep vein thrombosis (DVT) or chronic venous insufficiency — they might recommend ultrasound imaging or duplex ultrasound examination. This painless test uses sound waves to visualize your superficial veins and deep veins, showing how blood moves and whether the vein valves are closing properly.
Sometimes, they’ll also use Doppler scanning tests, which can detect even small irregularities in blood flow — like blood pooling or early signs of superficial vein thrombosis.
| Diagnostic Tool | What It Checks | Why It Matters |
| Ultrasound imaging | Flow, valve function, blood clots | Detects DVT, vein disorder, or vein disease early |
| Doppler scan | Speed and direction of blood flow | Identifies backflow or blockage |
| Physical exam | Skin tone, swelling, warmth | Reveals inflammation or infection |
| Blood tests | Signs of autoimmune conditions or infection | Helps spot causes like Behçet’s disease or polymyalgia rheumatica |
3. Blood Tests for Inflammation or Autoimmune Clues

If vein inflammation persists or if there’s suspicion of something systemic, your doctor might order blood tests. Elevated markers like ESR or CRP can hint at hidden vascular diseases, including temporal arteritis, Giant cell arteritis, or even autoimmune flare-ups that affect your vascular system.
These tests also help rule out infections that could irritate vein walls or cause swelling — and sometimes guide treatment with anti-inflammatory medicines or blood-thinning medications if clotting risk is high.
🩸 Pro Tip: If you’re visiting a vein specialist for the first time, bring a quick note of your habits — caffeine, exercise, hydration, any new supplements, or medicines like blood-thinning drugs.
4. Home Remedies and Lifestyle Adjustments
If you’ve been staring at those raised hand veins, wondering whether to call a vascular specialist or just grab a cold compress — you’re not alone. Sometimes, sudden bulging veins in hands with pain don’t require medical procedures at all. They just need a little attention, a few habit shifts, and maybe some cooling patience.
Your vascular health is deeply connected to everyday things — how much water you drink, how you move, and even what you eat. Here’s how to support your vein walls, improve blood flow, and reduce that occasional vein inflammation naturally.
5. Hydration & Cooling: The First Line of Calm
Dehydration thickens the blood, raising blood pressure and making veins more visible. Simply drinking enough fluids (especially if you sweat a lot from physical activity or live somewhere hot) can help veins settle back under the skin.
A few quick tips:
- Sip water consistently through the day — not all at once.
- Add a pinch of Himalayan salt or electrolytes if you exercise frequently.
- Cool your hands under running water or use a cold towel to ease pain and tenderness after workouts.
6. Compression Sleeves: Gentle Pressure for Blood Flow
When blood pooling or mild swelling lingers, compression therapy can be surprisingly effective. Compression sleeves or stockings apply light pressure on superficial veins, improving blood flow back toward the heart and reducing vein pain and swelling.
They’re particularly useful if your job involves long hours of standing or repetitive hand use.
🩸 Pro Tip: Choose breathable compression gear — not too tight — and wear it during daytime activity rather than overnight. If the swelling worsens or skin feels hot, stop and consult a vein specialist.
7. Dietary Adjustments: Nourish from Within
What you eat can either strengthen or strain your vascular system. A balanced diet supports your vein valves, improves circulation, and reduces inflammation.
| Nutrient / Habit | Why It Helps | Examples & Sources |
| Vitamin C & Bioflavonoids | Support collagen in vein walls | Citrus, berries, bell peppers |
| Antioxidants | Reduce vascular inflammation | Green tea, spinach, blueberries |
| Magnesium & Potassium | Balance blood pressure and muscle tone | Bananas, nuts, avocados |
| Omega-3 fatty acids | Improve blood flow and reduce clot risk | Salmon, flaxseeds, chia seeds |
Try to cut back on sodium-heavy foods that cause fluid retention — which can make vein pain and swelling worse — and consider adding gentle herbs like turmeric or ginger for their natural anti-inflammatory benefits.
8. Movement & Elevation: Let Gravity Help You
If you sit for hours or do repetitive tasks, blood can stagnate in your upper extremities, leading to vein discomfort. Try this simple routine:
- Stretch or shake your hands every 30 minutes.
- Raise your hands above heart level for 10 minutes daily to reduce blood pooling.
- Alternate between cardio exercise and light resistance work to keep veins flexible and valves active.
🩸 Pro Tip: After long hours typing or gripping tools, gently massage your forearms with upward strokes. It boosts blood circulation, reduces micro-swelling, and relaxes muscle fibers around superficial veins.
Quick Reference Table
| Lifestyle Habit | Benefit for Veins | Practical Example |
| Stay hydrated | Prevents blood thickening & vein dilation | 8–10 glasses/day |
| Exercise in moderation | Enhances blood flow & vein valve strength | Mix cardio + rest days |
| Elevate hands | Reduces pressure & vein pooling | 10 mins daily |
| Balanced diet | Strengthens vein walls | Vitamin C, antioxidants |
| Manage stress | Lowers blood pressure spikes | Deep breathing, walks |
Medical Treatments and Therapies
Sometimes, sudden bulging veins in hands with pain don’t fade away with home remedies or lifestyle adjustments. When discomfort persists or veins start to harden, change color, or cause hand fatigue, it’s time to explore medical treatment options.
The good news? Modern vascular medicine offers plenty of gentle, minimally invasive therapies that can ease symptoms, restore proper blood circulation, and even improve appearance.
1. Diagnosis: The First Step Toward Relief
Before jumping into treatment, a vascular specialist or phlebologist will typically perform a physical exam and may recommend an ultrasound scan. This imaging test checks for:
- Blood flow direction (to rule out valve damage)
- Clots or obstructions in deeper veins
- Signs of venous insufficiency or varicose vein formation
Depending on your results, the doctor can tailor a plan — from medication to small procedures — to restore normal vein function.
🩸 Pro Tip: Bring notes about when your hand vein pain worsens — after exercise, heat exposure, or rest. This helps pinpoint whether it’s vascular, muscular, or nerve-related.
2. Non-Surgical Treatments
For many, these simple medical therapies are enough to manage the issue without surgery:
| Treatment | How It Works | Ideal For | Recovery Time |
| Sclerotherapy | Injects a mild solution that collapses and fades damaged veins | Visible superficial veins, mild varicose veins | 1–3 days |
| Laser Therapy | Uses light to seal off spider or varicose veins | Shallow, surface-level veins | Minimal downtime |
| Compression Therapy | Improves blood flow and reduces vein pressure | Mild pain or swelling | Immediate, ongoing |
| Medication (anti-inflammatories, vein tonics) | Reduces pain, swelling, and vein wall inflammation | Vein tenderness or inflammation | Varies |
These treatments are often performed right in a clinic, without anesthesia, and are safe for most adults.
3. Surgical or Advanced Procedures
If your sudden bulging veins in hands are linked to chronic venous insufficiency, deep vein thrombosis, or severe valve damage, surgical options may be considered.
Here are a few possibilities:
- Vein Ligation and Stripping: Removes or ties off severely damaged veins.
- Ambulatory Phlebectomy: Extracts bulging surface veins through tiny incisions.
- Endovenous Laser Ablation (EVLA): Seals off faulty veins using laser energy under local anesthesia.
🩺 These procedures are typically reserved for persistent pain, skin discoloration, or restricted hand mobility — not just for cosmetic concerns.
4. Recovery and Prevention Tips
After any vein treatment, doctors usually recommend:
- Wearing compression sleeves for a few days.
- Keeping your hands elevated when resting.
- Avoiding strenuous weightlifting or heat exposure for at least a week.
- Drinking plenty of fluids to maintain blood flow and reduce swelling.
💡 Pro Tip: Post-treatment, add circulation-friendly foods like beets, garlic, and citrus fruits to your meals. They naturally support vascular healing and reduce inflammation.
When to See a Doctor and Warning Signs
While many cases of sudden bulging veins in hands with pain are harmless and linked to temporary factors like exercise or heat, there are times when those veins are your body’s way of saying — “Hey, something deeper’s going on.” Knowing when to seek medical advice can help you prevent complications and keep your vascular health on track.
1. Recognizing the Red Flags
Not every visible vein needs medical attention, but if you notice any of the following, it’s time to get checked by a vascular specialist or phlebologist:
🚨 Major Warning Signs:
- Persistent pain or burning sensation in the veins
- Swelling or puffiness around the hand or wrist
- Veins that stay enlarged for weeks even at rest
- Skin discoloration (bluish, purplish, or reddish tone)
- Hard or rope-like veins that feel tender to touch
- Warmth or red streaks over a vein (possible sign of thrombophlebitis)
- Numbness or tingling in the fingers (potential circulation issue)
If any of these symptoms appear suddenly — especially if accompanied by shortness of breath or chest pain — seek emergency care immediately. These could signal a deep vein thrombosis (DVT) or another serious vascular complication.
Normal vs Concerning Vein Changes
| Condition / Observation | Likely Benign Cause | Possible Medical Concern |
| Veins bulge after a workout | Increased blood flow & muscle pump | Persistent bulging without exercise |
| Veins visible in hot weather | Temporary vasodilation | Painful swelling or color changes |
| Mild hand ache | Overuse, dehydration | Throbbing or heat along vein |
| Visible vein + redness | Normal post-exercise flush | Inflamed vein (phlebitis) |
| Raised veins + numb fingers | Temporary tightness or tension | Circulatory restriction or nerve compression |
🩸 Pro Tip: If veins look more pronounced on one hand only — and the other appears normal — that’s an important clue to mention to your doctor. It could signal a localized blockage or vein valve problem.
2. What the Doctor Might Check
When you visit a clinic, a vein specialist will typically:
- Review your medical history and any family record of varicose or vascular disease.
- Examine your hand veins while at rest and after light activity.
- Conduct an ultrasound or Doppler study to check blood flow patterns.
- Test for venous reflux, thrombosis, or valve malfunction if symptoms persist.
If the pain or bulging is related to an underlying issue like phlebitis, thrombosis, or connective tissue disorder, early detection is key — it can prevent long-term circulation problems and protect your hand function.
💡 Pro Tip: Keep a small symptom diary before your visit — note the time of day, triggers (like heat, workouts, or stress), and any swelling or tingling. Doctors love having that data; it helps them pinpoint causes faster.
Myths vs. Facts About Bulging Veins
It’s funny how something as simple as visible veins can stir up so many misconceptions. One moment, someone’s telling you it’s from “too much exercise,” and another insists it’s a sign of poor health. The truth — as always — lives somewhere in between.
When you start noticing sudden bulging veins in hands with pain, it’s easy to spiral through a web of internet theories. But let’s sort through a few of the most common myths (and what science actually says).
🕸️ Common Myths and What’s Really True
| Myth | Reality (What’s Actually Happening) |
| “Bulging veins mean poor circulation.” | Actually, visible veins often mean good circulation. It’s when blood flows faster — during workouts or heat — that veins rise closer to the skin. Only when accompanied by pain or swelling might it hint at a vascular issue. |
| “Only older people get bulging veins.” | Age plays a role, sure — but genetics, body fat, muscle tone, and even temperature shifts can make veins stand out in young adults too. Athletes often have more visible veins because of lower subcutaneous fat and high blood flow. |
| “Bulging veins can be treated with creams.” | No topical cream can fix damaged vein valves or blood pooling. Some may improve skin tone or reduce redness, but deeper vein disease needs targeted care — like sclerotherapy, compression therapy, or Endovenous Laser Ablation. |
| “Bulging veins are always varicose veins.” | Nope. Varicose veins are twisted, enlarged, and often painful — but not every visible vein qualifies. Sometimes they’re just superficial veins responding to heat, stress, or dehydration. |
| “You can’t do anything to prevent them.” | You actually can. Healthy circulation habits, proper hydration, compression sleeves, and seeing a vascular specialist early can prevent chronic venous insufficiency or vein inflammation from getting worse. |
🌿 What the Science Says (and Doesn’t)
Veins don’t just “pop up” randomly. There’s always some physiological reason — from increased blood flow and low body fat to weakened vein walls or valve malfunction.
But what’s tricky is that it’s rarely just one factor. For instance, superficial vein thrombosis can mimic a temporary bulge caused by dehydration, while stress-related blood pressure spikes can trigger similar visible patterns.
So, before jumping to conclusions or slathering on another “vein cream,” try observing:
- Does it happen more when you’re hot or anxious?
- Do your hands feel tender, warm, or tingly?
- Does elevation or compression therapy help?
If yes, it’s worth mentioning to a vein specialist — not necessarily because it’s dangerous, but because it tells you something about your vascular system’s resilience.
🩸 Pro Tips from Vascular Experts
- Don’t panic over visibility. Veins show up more in lean, fit people. It’s often a sign of strong circulation — not disease.
- Check for patterns, not moments. A one-time flare-up is usually harmless; recurring pain, swelling, or skin changes deserve attention.
- Keep your hydration and posture in check. Even mild dehydration thickens blood and makes superficial veins appear larger.
- Avoid self-treating with random “miracle” gels. Look for clinically backed treatments like sodium tetradecyl sulfate injections, radiofrequency ablation, or ambulatory phlebectomy if needed — but only under medical advice.
💡 Pro Tip: The Cleveland Clinic and North Shore Vein Center recommend early screening if you notice persistent vein tenderness or color changes. Early ultrasound imaging can detect subtle valve issues long before symptoms worsen.
When to See a Specialist: Don’t Ignore These Red Flags
Sometimes, your veins are just doing what veins do — responding to temperature, movement, or stress. But other times, that sudden, throbbing bulge or deep ache isn’t just about appearance. It’s a message from your body saying, “Something’s off.”
If you’ve noticed sudden bulging veins in hands with pain that persist or come with unusual symptoms, it may be time to check in with a vascular specialist or vein doctor.
🩸 1. Persistent Pain or Swelling
A little soreness after exercise or a hot shower? Normal.
But if you’re feeling persistent vein pain, tenderness, or warmth that lingers for days — especially if the area feels rope-like or hardened — it could indicate vein inflammation (phlebitis) or even superficial thrombophlebitis. These occur when a blood clot forms close to the skin, blocking flow in a superficial vein.
Pro Tip: If swelling increases overnight or you wake up with a stiff, throbbing hand, don’t brush it off — it’s worth scheduling an ultrasound examination to rule out a deep vein thrombosis (DVT) in the upper extremities.
🔥 2. Skin Color or Temperature Changes
Your veins shouldn’t feel like hot wires under your skin.
If one hand looks redder, bluer, or more swollen than the other, or if you notice patches of heat and discoloration, it could mean poor blood flow or vascular inflammation.
When left unchecked, this can evolve into chronic venous insufficiency — where vein valves fail to close properly, allowing blood pooling and tissue damage.
| Symptom | Possible Concern | Why It Matters |
| Blue or purple veins + warmth | Superficial vein thrombosis | Early clot or inflammation |
| Red streaks along vein | Infection or phlebitis | Needs medical treatment |
| Cold, pale skin | Circulatory restriction | May signal a vascular blockage |
| Brownish or dark skin patches | Chronic venous disease | Indicates ongoing blood pooling |
💡 Pro Tip: Note which hand feels warmer or looks darker. That asymmetry helps doctors pinpoint whether the issue is localized vein trauma or a deeper vascular disorder.
⚠️ 3. Numbness, Tingling, or Weak Grip
If pain comes with numbness or tingling, especially in the fingers, it could suggest restricted blood flow or even nerve compression due to vein swelling.
Persistent tingling might also occur if blood pressure spikes or if there’s pressure buildup from inflammation in the vein walls.
🧠 4. Recurrent or Migrating Vein Pain
When bulging veins show up in different spots — say, one week near your wrist and the next near your forearm — it’s not random. Some conditions like Behçet’s disease or autoimmune inflammation can trigger these migrating vein flares.
If you’ve had recurrent episodes of hand vein pain, vein tenderness, or swelling, mention it to your vascular surgeon or rheumatologist. They may run blood tests or imaging scans to check for systemic vascular issues.
🩺 Doctor’s Checklist: What to Bring to Your Appointment
| What to Track Beforehand | Why It Helps Your Specialist |
| When bulging or pain started | Identifies triggers and frequency |
| Activities before symptoms | Links between exercise, heat, or stress |
| Color/temperature changes | Determines blood flow irregularities |
| Any medications or supplements | Checks for blood-thinning interactions |
| Family history of vein issues | Detects genetic vascular tendencies |
🩹 5. When It’s More Serious
You should seek immediate medical care if:
- Pain spreads beyond your hand to your arm or chest
- You feel short of breath or lightheaded
- Veins look dark, swollen, or tender to touch
- There’s a sudden loss of sensation or hand weakness
These can signal conditions like pulmonary embolism, venous thromboembolism, or other vascular diseases that require urgent attention.
Even though it sounds intense, seeing a vascular specialist early doesn’t always mean invasive procedures. Many cases resolve with compression therapy, anti-inflammatory medicine, or endovenous ablation therapy — minimally invasive and highly effective.
Sometimes, reassurance from a professional is all you need to stop worrying about every little pulse under your skin.
Conclusion
When it comes to sudden bulging veins in hands with pain, the key isn’t fear — it’s awareness. Your veins respond to the rhythm of your life: movement, heat, hydration, and even emotion. Sometimes, the changes you notice are temporary; other times, they’re gentle reminders that your circulatory system needs a little extra love. Learning to read these signs early helps you act with calm curiosity rather than panic.
So, the next time you see or feel something unusual — like swelling, warmth, or tenderness — treat it as a signal rather than a setback. Small lifestyle shifts such as staying hydrated, elevating your hands after long hours, and avoiding excessive strain can make a real difference. And if the discomfort lingers, consulting a vein specialist isn’t overreacting — it’s being proactive about your health.
Ultimately, your veins are storytellers of your body’s journey. Each pulse and pathway reflects balance, effort, and emotion. Paying attention to sudden bulging veins in hands with pain isn’t vanity — it’s self-respect. Listen to those signals, respond with care, and remember that your body always tries to communicate — you just have to learn its language.
Frequently Asked Questions
1. Why do I suddenly see bulging veins in my hands?
Sudden bulging veins in hands with pain can appear due to temperature changes, intense exercise, or dehydration. When blood circulation increases, veins expand to release heat or handle extra flow. But if they stay swollen or ache, it might point to vein inflammation or chronic venous insufficiency.
2. Can stress cause hand veins to bulge?
Yes, indirectly. Stress affects your vascular system — raising heart rate and blood pressure — which can cause superficial veins to dilate. Over time, this may make your veins more noticeable, especially in people with thin skin or lower fat in their hands.
3. How do I know if my bulging veins are normal or a sign of disease?
If the swelling fades after rest, it’s usually harmless. But if your veins stay enlarged, feel warm, or come with pain or redness, you might be dealing with thrombophlebitis (a type of vein inflammation) or early varicose vein formation. A vein specialist can confirm it through an ultrasound.
4. Can dehydration make veins in my hands more visible?
Absolutely. When you’re dehydrated, blood volume drops, and veins appear more pronounced. Combine that with warm weather or physical activity, and you’ll often see those rope-like veins stand out even more. Rehydration usually helps.
5. What medical conditions cause painful hand veins?
Conditions like superficial thrombophlebitis, varicose veins, vascular disease, and venous insufficiency can make hand veins painful or swollen. Occasionally, blood clots or inflammation of vein walls are involved — especially if there’s redness or tenderness.
6. Should I worry if only one hand has bulging veins?
If one hand looks swollen or feels warmer than the other, it might signal localized vein inflammation or a circulatory issue in that limb. It’s best to get it checked, especially if the pain is persistent or the veins look bluish and firm.
7. Can exercise make my hand veins bulge permanently?
Yes, for some people. Intense or weight-based workouts increase blood circulation and muscle growth, pushing veins closer to the skin’s surface. It’s a normal adaptation, not a disease. But if veins ache or burn, take a rest day — your body might be asking for balance.
8. When should I see a vein specialist?
Visit a vascular doctor if your hand veins are bulging and painful for more than a few days, if there’s discoloration, or if you notice hard, rope-like lines under the skin. Early diagnosis prevents complications like vein inflammation or venous reflux.
9. Can home remedies help with painful hand veins?
Yes, mild cases often improve with elevation, cold compresses, hydration, and stretching. Natural anti-inflammatory foods (like turmeric, garlic, and ginger) may also support vascular health. But persistent vein pain or swelling should always be checked medically.



