Living with ulcerative colitis isn’t just about handling flare-ups — it’s also about figuring out how every meal might affect you. That daily back-and-forth with food is what makes the question “What Are the Worst Foods for Ulcerative Colitis” so important.
And here’s the tricky part: the answer isn’t the same for everyone. While one person struggles with dairy, another might be fine but reacts badly to spicy foods or whole grain cereals. The patterns are there, though, and certain meals are repeat offenders when it comes to flare-ups.
That’s why this guide takes a closer look at What Are the Worst Foods for Ulcerative Colitis, breaking down the top culprits and offering realistic swaps. Whether you’re navigating a low-residue diet, testing the FODMAP approach, or simply trying to avoid daily triggers.
You’ll find clear, practical insights here. By the end, you’ll know not just what to cut back on, but also how to shape a diet that feels sustainable for you.
Understand What Are the Worst Foods for Ulcerative Colitis
Ulcerative colitis (UC) is a type of chronic inflammatory bowel disease. It mainly affects the lining of your colon, leading to irritation, ulcers, and the kind of pain that’s hard to explain unless you’ve felt it.
And while medication plays a big role in controlling the condition, diet is often the silent partner — for better or worse.
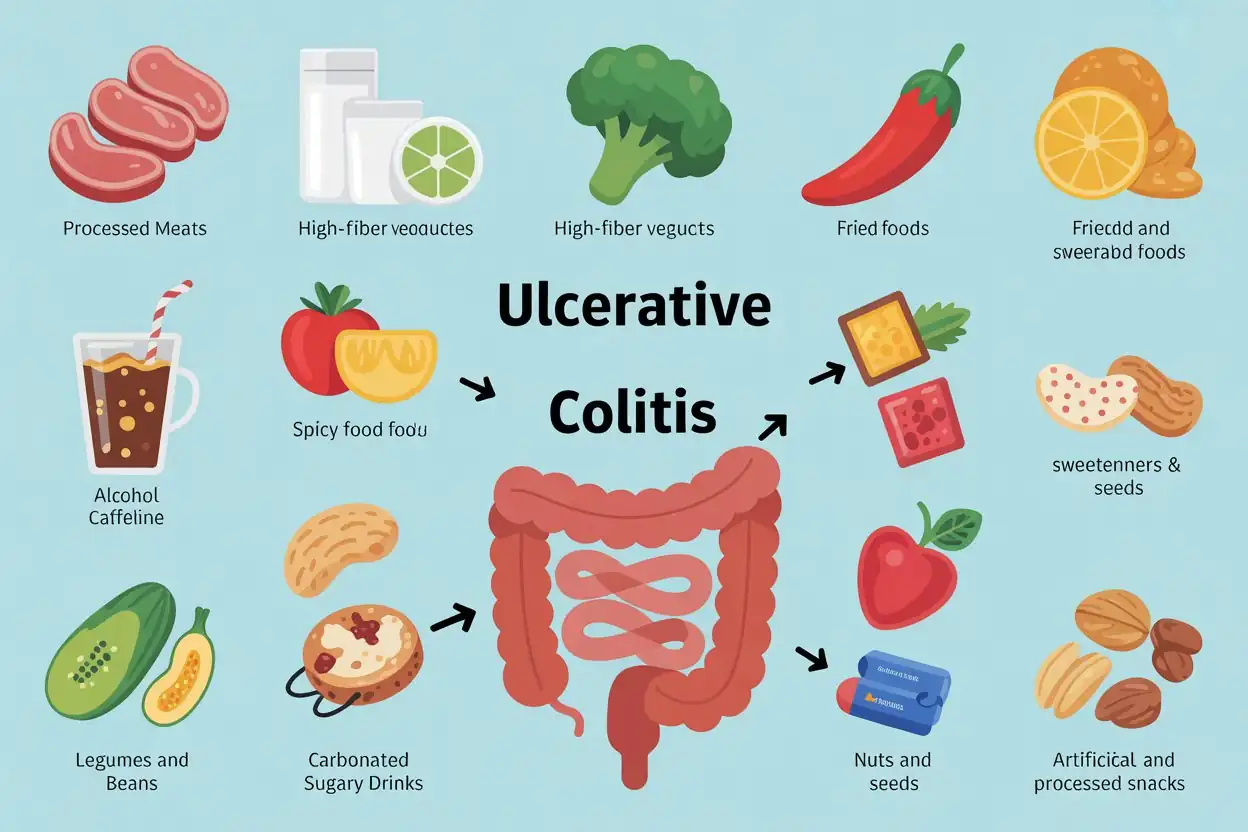
You’ve probably heard the phrase “food doesn’t cause UC, but it can worsen it.” That’s where the whole idea of what are the worst foods for ulcerative colitis comes in. Because it’s not about blaming a single trigger — it’s about recognizing patterns:
- High-fat diet choices (fried foods, fatty meats) that make digestion sluggish.
- Ultra-processed foods with additives and preservatives that irritate the gut.
- Sugary foods and drinks that spike inflammation and diarrhea.
- High-fiber foods (especially raw vegetables and legumes) that increase bloating and urgency.
- Carbonic acid in sodas that adds gas to an already sensitive system.
It’s tricky, because what’s “bad” for one person might be tolerable for another. Someone on a specific carbohydrate diet might completely cut out grains, while another person leans into a gluten-free diet only when symptoms flare.
Some folks explore the low-residue diet during severe flares, while others experiment with the Mediterranean diet or even omega-3 fatty acids to calm inflammation.
Pro Tip: Don’t just guess. If you’re unsure which ulcerative colitis diet triggers apply to you, start an elimination diet for two weeks. Reintroduce one food at a time. Patterns show up quickly — you’ll know what pushes your body toward UC flare-up foods and what keeps things relatively calm.
1. Processed Meats

Why Processed Meats Worsen UC
If there’s one category that almost always shows up on the “what not to eat” lists, it’s processed meats. And honestly, it makes sense. These foods are loaded with preservatives, sodium, nitrates, and saturated fats — all the little troublemakers that can stir up inflammation in the colon.
For someone already dealing with ulcerative colitis or other inflammatory bowel diseases, it’s like pouring gasoline on a fire.
Studies even suggest that a high-fat diet rich in deli meats and bacon may increase the risk of flare-ups compared to diets leaning toward omega-3 fatty acids or a Mediterranean-style diet.
And the problem isn’t just fat — it’s the additives in ultra-processed foods that confuse the gut microbiome, making symptoms like diarrhea, urgency, and cramping worse.
Examples to Avoid
- Sausages and hot dogs (especially the cheap, highly processed ones)
- Bacon (sorry… yes, even the crispy kind)
- Deli meats like ham, salami, or turkey slices with preservatives
- Canned meat products (corned beef, Spam, etc.)
It doesn’t mean all meat is off the table. Lean proteins like grilled chicken, turkey breast, or even certain types of fish rich in omega-3 fatty acids (like salmon or sardines) can be much safer options.
Pro Tip: If you’re craving that smoky flavor, try grilling or baking fresh chicken with herbs. You’ll get the savory satisfaction without the preservatives that make processed foods a UC nightmare.
2. Dairy Products

Lactose Intolerance and UC
Dairy is tricky. For some people with ulcerative colitis, a small splash of milk in coffee might be fine. For others, it’s an instant ticket to bloating, cramps, and diarrhea. The reason? Lactose intolerance is more common among those with chronic inflammatory bowel disease, meaning your gut just doesn’t break down milk sugar efficiently.
When lactose lingers undigested, it ferments, producing gas and irritation — not exactly what you want during a UC flare-up. And it’s not just milk. Creamy cheeses, yogurt with added sugar, and ice cream can all sneak in as hidden ulcerative colitis diet triggers.
Safer Dairy Alternatives
Here’s a quick table that makes the choices clearer:
| Common Dairy | Why It’s a Problem | UC-Friendly Alternative |
| Whole milk | High lactose, harder to digest | Lactose-free milk, almond milk, oat milk |
| Ice cream | Fat + lactose overload | Coconut-based or lactose-free ice cream |
| Soft cheeses (brie, cream cheese) | Higher lactose content | Hard cheeses (cheddar, parmesan) in moderation |
| Yogurt with added sugar | Lactose + sugar spike | Plain lactose-free or plant-based yogurt |
Switching to a gluten-free diet isn’t always necessary for UC, but dairy swaps can sometimes feel like a lifesaver when combined with a low-residue diet or a bland diet during flare-ups.
3. High-Fiber Vegetables

Fiber Types That Irritate UC
It feels counterintuitive, right? What are the worst foods for ulcerative colitis Vegetables are healthy — we’ve been told that forever. But with ulcerative colitis, especially during flare-ups, high-fiber foods can be one of the sneakiest triggers.
Insoluble fiber, the rough kind found in raw carrots, broccoli, or whole grain cereals, can be too abrasive for an inflamed colon. Instead of soothing digestion, it scratches at it, sometimes causing cramps, bloating, or even diarrhea.
This doesn’t mean vegetables disappear from your life. It’s more about how they show up on your plate. During calm periods, some people manage small portions of cooked veggies as part of a Mediterranean diet or even a low-FODMAP diet. But when UC flare-up foods are in question, raw high-fiber vegetables often top the list of what to avoid.
Cooking Tips to Reduce Irritation
- Peel the skins off veggies (skins are fiber-heavy).
- Steam or boil vegetables until soft — less work for your gut.
- Puree soups or mash vegetables for easier digestion.
- Avoid raw salads during flare-ups; stick to well-cooked options.
Some patients also experiment with a low-residue diet or bland diet during rough patches. Both approaches temporarily reduce fiber to give the gut a break.
Pro Tip: Keep a food journal. If zucchini in soup works but raw spinach salad doesn’t, jot it down. Over time, you’ll build your own ulcerative colitis exclusion diet without relying on generic lists.
4. Spicy Foods

Capsaicin’s Role in Irritation
If you’ve ever had a chili pepper set your mouth on fire, imagine what capsaicin — the active compound in spicy foods — does to an already inflamed colon. For many people with ulcerative colitis, spicy meals are a direct route to urgency, abdominal pain, and sometimes even worse diarrhea and you did not even understand what to eat when you have diarrhea.
The irritation isn’t just about heat; it’s about stimulation. Capsaicin can make the intestinal lining more sensitive, which is the last thing you need if you’re dealing with chronic inflammatory bowel disease.
And it’s not only obvious foods like hot sauce — even dishes that seem mildly seasoned, like spicy curries, may sneak into the “worst foods for colon inflammation” category.
Moderation Tips
- If you’re experimenting, start with milder spices (like turmeric or ginger) instead of chili flakes.
- Eliminate hot sauces temporarily if you’re in the middle of a flare.
- Focus on flavor layering: herbs (basil, parsley, rosemary) can give food depth without triggering UC flare-up foods.
Some people find that bland diets or Mediterranean-style diets with herbs instead of heat help reduce irritation while still making food feel enjoyable.
Pro Tip: If you miss the “kick,” try citrus zest or a splash of vinegar for brightness. It’s not the same as chili heat, but it adds flavor without stirring up symptoms.
5. Fried and Fatty Foods

Why Fatty Foods Trigger Symptoms
Here’s where things get complicated: fat isn’t the enemy, but too much of the wrong kind absolutely is. A high-fat diet packed with fried foods, creamy sauces, or greasy takeout can overwhelm digestion, slowing things down in all the wrong ways.
For someone with ulcerative colitis — or any chronic inflammatory bowel disease — that sluggish digestion can translate to bloating, cramps, and, well, too many trips to the bathroom.
The bigger issue is inflammation. Saturated fats, especially from fried foods or fatty meats, have been linked with worse UC symptoms. Compare that to omega-3 fatty acids from fish or even a Mediterranean-style diet that emphasizes olive oil — those fats may actually calm inflammation instead of fueling it.
Healthier Alternatives
If fried chicken and French fries are on your “comfort list,” you don’t have to give them up forever. It’s more about finding safer swaps that don’t act like UC flare-up foods:
- Grilled or baked chicken instead of deep-fried.
- Air-fried potatoes instead of greasy fries.
- Olive oil or avocado oil instead of butter or lard.
- Fatty fish (salmon, sardines) as a source of omega 3 fatty acids.
| Problematic Choice | Why It Irritates UC | Safer Swap |
| Fried chicken | High-fat, greasy coating | Grilled or oven-baked chicken |
| Fast-food burgers | Ultra-processed foods + fatty meat | Lean turkey or veggie burger (if tolerated) |
| Heavy cream sauces | Saturated fat overload | Olive oil–based dressings |
| French fries | Greasy, ultra-processed snack | Air-fried or baked potato wedges |
Pro Tip: If you’re craving fried foods, try the air fryer. It gives the crisp without drowning your food in oil — way easier on a sensitive gut.
6. Alcohol and Caffeine

Irritating Effects on the Colon
Alcohol and caffeine are two of the most common ulcerative colitis diet triggers, though plenty of people experiment with “just a little” and see what happens. The problem is they both stimulate the digestive tract — sometimes too much.
- Alcohol can increase inflammation and, in some cases, even bleeding. Wine, beer, and cocktails with mixers are especially rough because they often combine alcohol with sugar or carbonated drinks (two other UC troublemakers).
- Caffeine, meanwhile, speeds things up. Coffee, strong tea, and energy drinks can trigger urgency and diarrhea — not exactly ideal during a flare.
Safer Consumption Practices
This doesn’t mean you’re doomed to a life without coffee or the occasional celebratory toast. But moderation and mindful swaps are key:
- Switch to decaf coffee or tea during flares.
- Try herbal teas (peppermint, chamomile) that soothe instead of stimulate.
- Explore alcohol-free alternatives like mocktails, sparkling water with citrus, or non-alcoholic beers (though check for carbonation).
- If you do drink alcohol, choose a small glass of wine with food instead of beer or cocktails.
Pro Tip: If you can’t resist coffee, pair it with food. Drinking it on an empty stomach is more likely to trigger UC flare-up foods, while having it alongside a bland breakfast (like oatmeal or eggs) can sometimes soften the impact.
7. Carbonated and Sugary Drinks

Gas, Bloating, and Sugar Spikes
If there’s one category of “everyday indulgence” that people underestimate, it’s drinks. Sodas, energy drinks, sweetened juices carbonated soft drinks — they’re everywhere, but for ulcerative colitis they can be brutal.
Carbonated drinks are loaded with carbonic acid, which adds extra gas to the digestive tract. For someone already prone to bloating, it’s like pumping air into an already stretched balloon.
Then there’s sugar. Sugary foods and drinks can spike blood sugar and irritate the gut microbiome, increasing inflammation and worsening diarrhea. Even fruit juices (the “healthy” kind) can sneak into the worst foods for colon inflammation because of their high fructose load.
And don’t forget artificial sweeteners — sorbitol and maltitol in “diet” sodas or sugar-free products can be just as irritating.
Healthier Beverage Choices
- Herbal teas like chamomile, peppermint, or ginger (often soothing).
- Plain water — always the safest baseline.
- Electrolyte drinks without sugar (look for ones with minimal additives).
- Diluted fruit juices (apple or grape, watered down) for those who still want flavor.
| Problematic Drink | Why It’s a Trigger | Safer Alternative |
| Soda / cola | Carbonic acid + sugar overload | Herbal tea, sparkling water (if tolerated) |
| Energy drinks | Caffeine + sugar + carbonation | Decaf iced tea or electrolyte water |
| Fruit juice (undiluted) | High fructose load | Diluted juice or smoothies with low-FODMAP fruits |
| Diet sodas | Artificial sweeteners (sorbitol, maltitol) | Infused water (mint, cucumber, citrus) |
Pro Tip: If you miss the fizz, try sparkling water — but cautiously. Some UC patients tolerate it, others find the bubbles too much. Keep a food journal to see which camp you fall into.
8. Legumes and Beans
High Fiber and Gas Production
Beans, lentils, chickpeas — all staples of plant-based eating — are tricky for anyone managing a chronic inflammatory bowel disease. The problem isn’t just their fiber content (though that’s big).
It’s also the complex sugars in legumes that ferment in the gut, producing gas and bloating. That combination can turn a seemingly healthy lentil soup into a UC flare-up trigger.
Legumes are often listed on elimination diet charts, especially during flares, because of their tendency to irritate the colon. Even on a low-FODMAP diet, many beans are flagged as problematic. That doesn’t mean they’re off-limits forever, but they’re definitely in the “handle with care” column.
Preparation Tips
- Soak beans overnight — reduces some of the fermentable sugars.
- Puree beans into soups to make them gentler on digestion.
- Try smaller portions (like a few spoonfuls) instead of a whole bowl.
- Experiment with low-FODMAP legumes such as small amounts of canned lentils or chickpeas (rinsed thoroughly).
| Legume / Bean | UC Risk Level | Notes |
| Kidney beans | High | Gas-producing, fiber-dense |
| Chickpeas | Medium | May be tolerated in hummus form |
| Lentils (red/green) | Medium | Easier if well-cooked and pureed |
| Black beans | High | Very fermentable sugars |
| Canned lentils | Lower | Rinsing reduces fermentable carbs |
Pro Tip: If you’re trying to add more plant protein, start with smooth hummus or red lentil soup. Both are gentler than a bowl of whole beans.
9. Nuts and Seeds

Digestive Irritation Risks
Here’s the thing: nuts and seeds are nutrient powerhouses — full of healthy fats, protein, and even omega-3 fatty acids. But when your colon is inflamed, those tiny, hard-to-digest bits can feel like sandpaper.
For many with ulcerative colitis, especially during flare-ups, whole nuts and seeds end up on the “ulcerative colitis foods to avoid” list. It’s not that they’re inherently bad.
The rough textures and insoluble fiber can irritate the gut lining, making urgency, bloating, or diarrhea worse. That’s why many ulcerative colitis exclusion diets, bland diets, and even low-residue diets recommend skipping them — at least in their whole form.
Safer Consumption Methods
- Nut butters (peanut, almond, cashew) — smooth and easier to digest.
- Finely ground seeds (like flaxseed meal or chia blended into smoothies).
- Small portions only — not handfuls.
- Soaked chia or flax (creates a gel that’s gentler on the gut).
| Whole Nuts/Seeds | Why They Irritate UC | Safer Alternative |
| Almonds (whole) | Hard texture, high insoluble fiber | Almond butter |
| Sunflower seeds | Seed shells irritate lining | Ground sunflower seed butter |
| Chia seeds (dry) | Expand and cause bloating | Soaked chia gel |
| Flax seeds (whole) | Pass undigested, irritating | Flaxseed meal |
Pro Tip: If you miss the crunch of nuts, try sprinkling finely ground flaxseed or hemp hearts over yogurt or oatmeal. You’ll get nutrients without rough textures that act like UC flare-up foods.
10. Artificial Sweeteners and Processed Snacks

Gut Irritation and Inflammation
Artificial sweeteners can be sneaky. They’re marketed as “sugar-free,” but for someone with ulcerative colitis, they’re often worse than the real thing. Sorbitol, maltitol, and other sugar alcohols can act like laxatives, pulling water into the colon and causing bloating, cramps, and diarrhea.
That’s why “sugar-free gum” or “diet desserts” often pop up on elimination diet charts as hidden UC triggers. Processed snacks — chips, cookies, packaged cakes — are no better. Ultra-processed foods combine additives, preservatives, and refined grains in ways that irritate the gut and spike inflammation.
In fact, some research suggests that people with inflammatory bowel diseases like Crohn’s disease and ulcerative colitis tend to fare worse on diets high in refined grains and low in whole, natural foods.
Healthier Snack Alternatives
- Fresh fruit (low-FODMAP options) like bananas or blueberries.
- Rice cakes or plain crackers (easy to digest, bland diet-friendly).
- Homemade treats using oats, lactose-free milk, or nut butter.
- Smoothies with low-FODMAP fruits and lactose-free yogurt.
| Problematic Snack | Why It Worsens UC | Safer Alternative |
| Sugar-free gum | Sorbitol causes diarrhea | Herbal tea, peppermint leaves |
| Potato chips | High fat + additives | Air-popped popcorn (if tolerated) |
| Packaged cookies | Refined grains + sugar | Homemade oat cookies |
| Candy bars | Sugar + processed fats | Dark chocolate (small amounts, if tolerated) |
Pro Tip: If you crave sweets, try frozen grapes or banana slices dipped in a little lactose-free yogurt. It satisfies the sugar craving without processed foods sneaking into your diet.
How to Reduce Flare-Ups While Eating Safely
What are the worst foods for ulcerative colitis? Living with ulcerative colitis often feels like a balancing act. On one hand, you want nutrient-rich meals; on the other, you need to avoid ulcerative colitis trigger foods that set off painful flare-ups. The goal isn’t just to know what not to eat — it’s also about creating a UC-friendly diet plan that supports healing and keeps inflammation at bay.
Practical Strategies
Here are a few approaches that many people with inflammatory bowel disease (IBD) find helpful:
- Follow a Low-Residue Diet During Flares
- Focus on soft, easy-to-digest foods like white rice, scrambled eggs, and cooked carrots.
- This reduces fiber and gives your gut a break while still fueling your body.
- Focus on soft, easy-to-digest foods like white rice, scrambled eggs, and cooked carrots.
- Try an Exclusion Diet to Identify Triggers
- Eliminate common UC trigger foods (like dairy, gluten, and spicy meals) for a few weeks.
- Gradually reintroduce one at a time to see what sparks symptoms.
- Eliminate common UC trigger foods (like dairy, gluten, and spicy meals) for a few weeks.
- Portion Control Matters
- Smaller, frequent meals are easier to tolerate than heavy plates that overwhelm digestion.
- Smaller, frequent meals are easier to tolerate than heavy plates that overwhelm digestion.
- Stay Hydrated
- Diarrhea and flare-ups can cause dehydration — plain water, broths, and oral rehydration solutions help.
- Diarrhea and flare-ups can cause dehydration — plain water, broths, and oral rehydration solutions help.
- Cook Smart
- Steaming, baking, or poaching foods preserves nutrients without adding inflammatory oils or additives.
- Steaming, baking, or poaching foods preserves nutrients without adding inflammatory oils or additives.
Example of a UC-Friendly Meal Plan
| Meal | Safe UC-Friendly Option | Why It Works |
| Breakfast | Scrambled eggs + oatmeal made with lactose-free milk | Gentle on digestion, low residue |
| Snack | Banana or smooth applesauce | Easy to digest, no rough fiber |
| Lunch | Grilled chicken + mashed potatoes + cooked carrots | Bland, low-fat, filling |
| Snack | Rice cakes with almond butter | Provides energy without heavy fiber |
| Dinner | Baked salmon + white rice + zucchini (peeled and cooked) | Anti-inflammatory omega 3s, gentle starches |
Pro Tip: Keep a food and symptom journal. Tracking what you eat and how your body responds makes it easier to identify ulcerative colitis foods to avoid without relying only on guesswork.
Conclusion
So, what are the worst foods for ulcerative colitis? Honestly, they’re the ones that poke at an already sensitive gut — processed meats, fried and fatty foods, spicy dishes, carbonated drinks, artificial sweeteners… the list goes on. But here’s the catch: no two people with chronic inflammatory bowel disease respond exactly the same way.
One person might handle dairy without issue, while another finds even a sip of milk sends them straight into a flare. The trick isn’t just avoiding UC trigger foods, it’s also building a diet that makes sense for your body.
That might mean leaning on a low-residue diet during rough patches, then slowly bringing in Mediterranean-style meals rich in omega-3 fatty acids during calmer periods. It could mean keeping a diet sheet or a food journal, noting patterns, testing out elimination diets, and circling back to safe staples when your system feels fragile.
If you remember nothing else, remember this: ulcerative colitis foods to avoid are only half the story — safe, soothing foods are just as important. And you don’t have to figure it all out alone. A dietitian or gastroenterologist can help you determine what are the worst foods for ulcerative colitis fine-tune a plan that fits your symptoms, your cravings, and your lifestyle.
People Also Ask (FAQ’s)
1. What are the 6 worst foods for ulcerative colitis?
Processed meats, fried foods, spicy dishes, high-fiber raw veggies, sugary drinks, and artificial sweeteners are common UC triggers. They tend to cause irritation, bloating, or even flare-ups because the colon is already sensitive.
2. What fruits can I eat with colitis?
Bananas, melons, and peeled or cooked apples are usually easier to digest than raw, fibrous fruits. Soft textures and low-fiber options are often safest during flare-ups.
3. Which food is not good for ulcerative colitis?
Anything ultra-processed, greasy, or high in insoluble fiber often worsens UC symptoms. Think of packaged snacks, fried fast foods, or raw cruciferous veggies like broccoli.
4. Is rice bad for ulcerative colitis?
White rice is generally soothing, while brown rice’s extra fiber can sometimes irritate flare-ups. Many people lean on plain rice as a gentle base during sensitive days.
5. What is the healthiest diet for ulcerative colitis?
Many do well on a Mediterranean-style diet or low-FODMAP plan, adjusted to personal tolerance. The key is balance — nourishing foods without the usual UC triggers.
6. What is the latest treatment for ulcerative colitis?
Biologic therapies and targeted small-molecule drugs are the newest options alongside traditional meds. These newer treatments aim to calm inflammation at its root, not just mask symptoms.
7. What are anti-inflammatory foods?
Salmon, olive oil, turmeric, and leafy greens are known for helping calm inflammation. They fit naturally into diets like the Mediterranean-style diet that many UC patients explore.
8. What is the miracle drug for ulcerative colitis?
There isn’t a single miracle drug — treatments vary, though biologics feel closest for some patients. Success usually depends on a mix of medication, diet, and lifestyle adjustments.
9. What is a good dinner for someone with colitis?
Grilled chicken, mashed potatoes, and steamed zucchini make a gentle, balanced UC-friendly meal. It’s filling without being too harsh on the digestive tract.
10. What can worsen ulcerative colitis?
Stress, infections, and trigger foods like alcohol, caffeine, and fried meals can all spark flares. Even lack of sleep or skipping meals can sometimes make symptoms worse.